POC Tests Evaluated for Filarial Antigenemia
By LabMedica International staff writers
Posted on 28 Sep 2017
Lymphatic filariasis (LF) is a major neglected tropical disease (NTD) that has been targeted for elimination by 2020. The Global Programme to Eliminate Lymphatic Filariasis (GPELF, launched in 2000) uses repeated rounds of mass drug administration (MDA) with antifilarial drugs to interrupt transmission of the parasite.Posted on 28 Sep 2017
Antigen testing is more sensitive for filarial infection than tests that detect microfilariae (Mf) in night blood. Point-of-care (POC) antigen tests can be performed with finger prick blood collected during the day or night, and they provide a visual result in 10 minutes. The performance of two POCs has been compared.
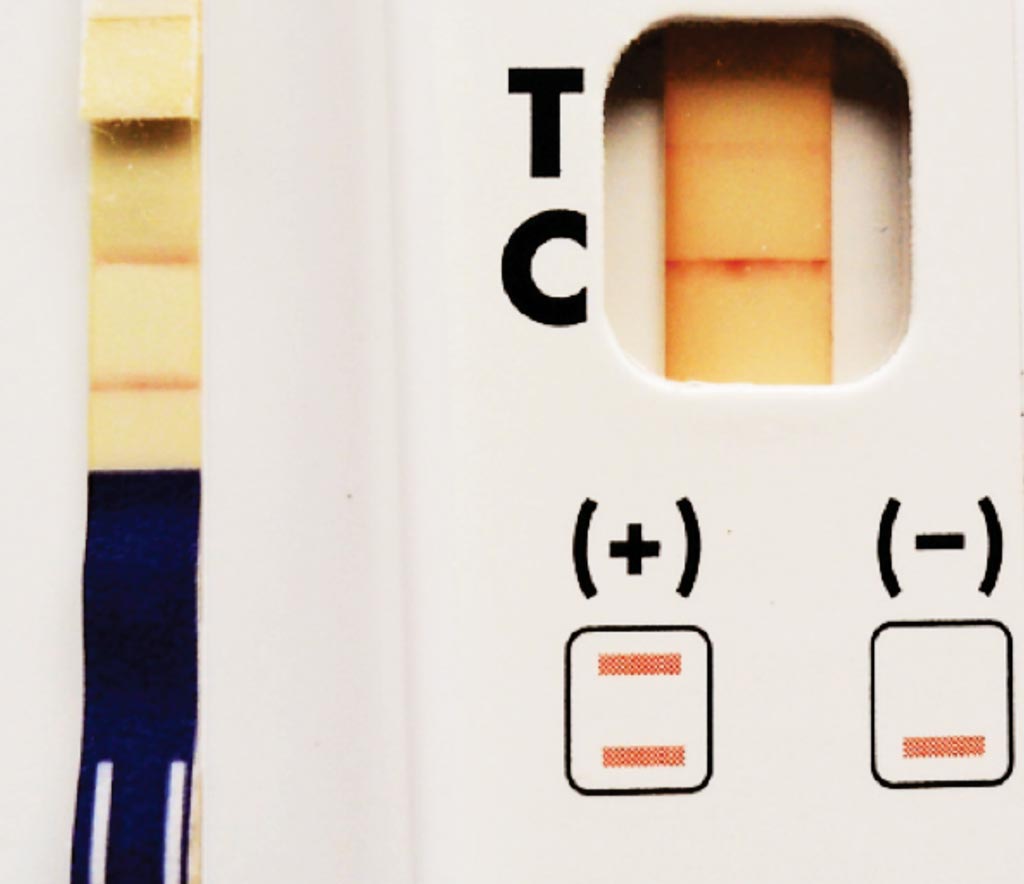
Image: The Alere Filariasis Test Strip (FTS) (Left panel, strong positive) and The BinaxNOW Filariasis Immunochromatographic card (Right pane, weak positivel) are in vitro immunodiagnostic tests used to detect Wuchereria bancrofti antigen in whole blood, serum, or plasma (Photo courtesy of Dr. Peter U Fischer).
An international team of scientists working with those at Washington University School of Medicine (Saint Louis, MO, USA) compared the tests prior to MDA in two study sites (Congo and Côte d'Ivoire) and in three sites that had received MDA (Democratic Republic of Congo and two sites in Liberia). Data were analyzed with regard to positivity, agreement and heterogeneity. Models evaluated potential effects of age, gender, and blood microfilaria (Mf) counts in individuals and effects of endemicity and history of MDA at the village level.
The two POCs tested were the BinaxNOW Filariasis Immunochromatographic card test (ICT), and the more recently introduced Alere Filariasis Test Strip (FTS) both from Alere. All individuals with positive ICT and/or FTS tests were asked to provide a second blood sample between 10:00 PM and 1:00 AM for assessment of Wuchereria bancrofti Mf. In West Africa, fingerprick blood was collected in capillary tubes with EDTA anticoagulant, and this blood was used to prepare Mf smears.
The team analyzed the test results from a total of 3,682 individuals. FTS test scores in persons with positive test results were often higher than ICT scores (46.3% in pre-MDA sites and 35.2% in post-MDA sites). Only 14 subjects (0.4%) were ICT-positive and FTS-negative. Eleven of these cases were from Côte d'Ivoire (pre-MDA), and four of the 12 individuals with this profile who provided night blood were microfilaremic. Antigenemia rates were 8% and 22% higher by FTS than by ICT in pre-MDA and in post-MDA sites, respectively. FTS/ICT ratios were higher in areas with low infection rates.
The authors concluded that their study provided extensive new information on the performance of the FTS compared to ICT in Africa and it has confirmed the increased sensitivity of FTS reported in prior studies. Variability in FTS/ICT was related in part to endemicity level, history of MDA, and perhaps to the medications used for MDA. These results suggest that FTS should be superior to ICT for mapping, for transmission assessment surveys, and for post-MDA surveillance. The study was published on September 11, 2017, in the journal Public Library of Science Neglected Tropical Diseases.
Related Links:
Washington University School of Medicine