Premature Birth Risk Linked to Bacteria in Cervicovaginal Space
By LabMedica International staff writers
Posted on 17 Feb 2017
Changes in microbial communities have been implicated in both health and disease and investigations into the association between the cervicovaginal (CV) microbiota and spontaneous preterm birth (SPTB) have been limited in scope and number.Posted on 17 Feb 2017
Premature or preterm birth, defined as that which occurs before 37 weeks of pregnancy, is the leading cause of death worldwide among children under five years of age. In 2015, around 1 in 10 babies born in the USA were premature; however rates of premature birth in the USA fell between 2007 and 2014, partly due to reductions in the number of births to teenagers and young mothers.
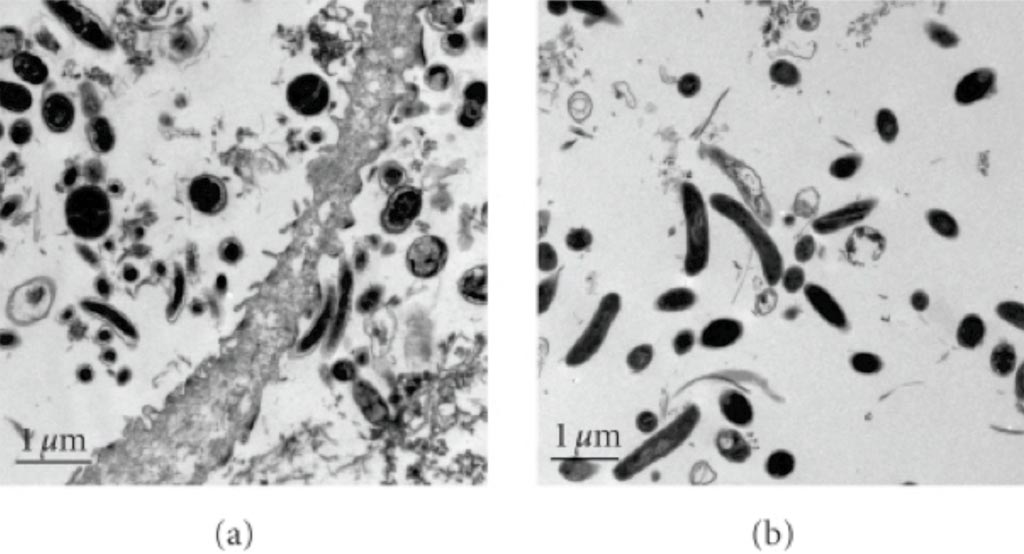
Image: (a) A scanning electron micrograph (SEM) of vaginal fluid from a woman with bacterial vaginosis and high concentrations of bacterial vaginosis associated bacterium 1 (BVAB1); (b) These cells are different from the larger, wider, and more electron dense curved rods observed in a pure culture of Mobiluncus curtisii (Photo courtesy of the US National Library of Medicine).
A team of scientists working with the Perelman School of Medicine examined the microbiota in vaginal swabs of 1,500 pregnant women sampled at three different times during pregnancy: during weeks 16-20, weeks 20-24, and weeks 24-28. A nested case-control was performed with 80 spontaneous preterm birth (SPTB) cases and 320 term controls that were frequency matched by race to the cases. 16S rRNA gene analyses were performed to characterize the composition and structure of the CV microbiota.
The investigators performed phylotype analyses, and 127 phylotypes were detected in all samples from both cohorts. Significant associations were demonstrated between specific bacteria, in both a positive and negative manner, with SPTB. The team found 37 bacteria were significantly associated with a decreased risk of SPTB while 13 were associated with an increased risk in the primary cohort. Racial differences in these associations were evident. The validation cohort confirmed the highly significant associations between specific microbes and SPTB. Bifidobacterium species were noted to be significantly protective against SPTB at all gestational time points while BVAB2, BVAB3 and Mobiluncus were associated with a dramatic increase risk of SPTB.
The authors concluded that CV microbiota are significantly associated with SPTB. Targeting the bacteria that are associated with an increased risk of SPTB and/or enhancing the presence of the protective bacteria may serve as new therapies to reduce the rate of PTB. An abstract of the study was published on January 26, 2017, in the American Journal of Obstetrics & Gynecology.









 Analyzer.jpg)