Rapid Adaptation of Aspergillus Presents Doctors with Dilemma
By LabMedica International staff writers
Posted on 14 Oct 2016
Aspergillus fumigatus causes a range of diseases in human beings, some of which are characterized by fungal persistence and the fungus can persist by adapting to the human lung environment through physiological and genomic changes.Posted on 14 Oct 2016
The physiological changes are based on the large biochemical versatility of the fungus, and the genomic changes are based on the capacity of the fungus to generate genetic diversity by spontaneous mutations or recombination and subsequent selection of the genotypes that are most adapted to the new environment.
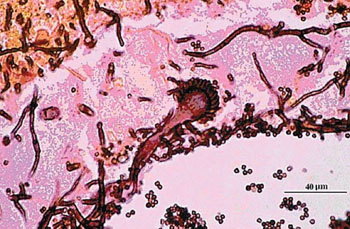
Image: A histology of Aspergillus fumigatus in lung tissue (Photo courtesy of the CDC).
Scientists at the Radboud University Medical Center (Nijmegen, Netherlands) and their colleagues suggest that any change can stimulate the fungus to adapt. This applies equally to starting a new treatment, substituting one antifungal medication for another or entirely stopping treatment. Knowing that all environmental changes can stimulate adaptation in the fungus poses a problem for doctors. Treating the fungus with medication could lead to drug resistance, but not treating the fungus or discontinuing the initial treatment makes it easier for the fungus to settle in the lungs. Either one of these options may make it difficult to eradicate the fungus from the patient.
The team explored the adaptation strategies of A. fumigatus in relation to azole resistance selection and the clinical implications thereof for management of diseases caused by Aspergillus spp. The emphasis of the study was what primarily affects lung patients who are long-term carriers of the Aspergillus fungus, such as patients with chronic obstructive pulmonary disease (COPD) or cystic fibrosis. Stress factors, such as triazole exposure, cause mutations that render resistance. The process of reproduction that is sexual, parasexual, or asexual, is probably crucial for the adaptive potential of Aspergillus spp. As any change in the environment can provoke adaptation, switching between triazoles in patients with chronic pulmonary aspergillosis might result in a high-level pan-triazole-resistant phenotype through the accumulation of resistance mutations. These results call for a modification of the current treatment guidelines.
A similar adaptation is expected to occur in response to other stress factors, such as endogenous antimicrobial peptides; over time the fungus will become increasingly adapted to the lung environment, thereby limiting the probability of eradication. The group’s hypothesis challenges current management strategies, and future studies should investigate the genomic dynamics during infection to understand the key factors facilitating adaptation of Aspergillus spp. The study was published on September 13, 2016, in the journal The Lancet Infectious Diseases.
Related Links:
Radboud University Medical Center