New UTI Diagnosis Method Delivers Antibiotic Resistance Results 24 Hours Earlier
Posted on 27 Dec 2025
Urinary tract infections affect around 152 million people every year, making them one of the most common bacterial infections worldwide. In routine medical practice, diagnosis often relies on rapid urine tests that detect nitrites and leukocytes, after which broad-spectrum antibiotics are frequently prescribed without identifying the exact pathogen. Laboratory-based antibiotic resistance testing is usually reserved for high-risk patients and can take two to three days, delaying targeted treatment. This gap leads to unnecessary antibiotic use, longer recovery times, and rising resistance, highlighting the need for faster and more precise testing. Now, a new urine-based testing approach speeds up antibiotic resistance detection for urinary tract infections.
The new diagnostic approach developed by researchers at Technical University of Munich (Munich, Bavaria, Germany; www.tum.de) comprises two methods that allow urine samples to be tested directly for antibiotic susceptibility, eliminating the need for labor-intensive bacterial pre-cultivation that is standard in laboratories. By skipping this step, the overall time required to determine antibiotic effectiveness is significantly reduced.
In the main method, urine is applied directly onto an agar plate containing antibiotic disks. The areas where bacterial growth is suppressed, known as inhibition zones, are then measured. A key innovation is an algorithm that factors in the actual bacterial concentration in urine and adjusts how this affects inhibition zone size, enabling reliable resistance profiling even without standardized bacterial suspensions.
The new test was validated by directly comparing its results with those from conventional laboratory methods. In these comparisons, the approach showed a correlation of approximately 94 percent with the standard reference method. The findings, published in a peer-reviewed scientific journal, indicate that the faster procedure can closely match established testing accuracy while delivering results up to 24 hours earlier.
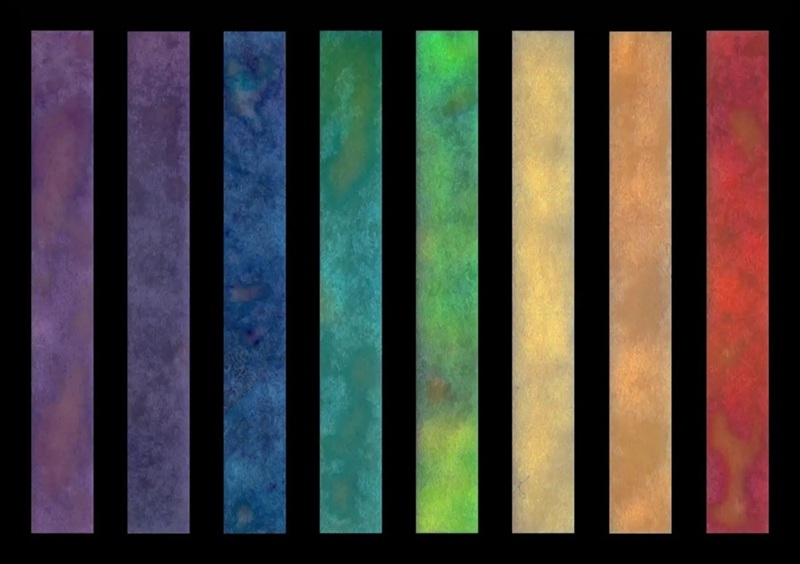
Researchers are now analyzing cases where results differ from the reference method, such as samples with very low bacterial counts or mixed infections, to further refine and improve the test’s performance. In parallel with the agar-based approach, the team is developing a paper-based point-of-care device built on similar principles. This version is designed to identify eight different bacterial species through color changes and to indicate antibiotic resistance, potentially enabling rapid decisions directly at the point of care.
Going forward, the researchers aim to create a compact, easy-to-use test suitable for routine medical practices and, eventually, home use. Future versions are expected to display results on a smartphone and be adaptable for low-resource settings, where fast and reliable diagnostics are especially critical.
“Our goal is a small, easy-to-use test that can be deployed in any medical practice with minimal effort and, in the future, also allows patients to test themselves at home using a paper-based device with results displayed on their smartphone,” said Henning Sabersky-Müssigbrodt, first author of the study. “The technology is designed so that it can also be applied in low-resource settings, where rapid and reliable diagnostics are particularly critical.”
Related Links:
Technical University of Munich