Elevated Interleukin-12/23p40 Indicates Dysfunctional Heart Rate Variability in T2D
Posted on 08 Feb 2022
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in type 2 diabetes (T2D), accounting for approximately 50% of all deaths. Cardiovascular functions, including heart rate, heart contractility, and blood pressure, are regulated by autonomic sympathovagal balance.
Inflammation is an underlying pathogenic component in T2D, along with hyperglycemia, hyperlipidemia, and hypertension, adding to endothelial dysfunction and accelerated atherosclerosis. Systemic inflammation is assessed by serum levels of proinflammatory cytokines such as tumor necrosis factor (TNF)‐α and interleukin (IL) such as IL‐6.
Medical Scientists at the Aalborg University Hospital (Aalborg, Denmark) and their colleagues analyzed serum samples from 100 participants with type 2 diabetes who were recruited consecutively between March 2018 and August 2020. Eligible participants were ≥ 18 years old, of Northern European descent, with verified T2D for more than 1 year (HbA1c ≥ 6.5%).
Serum concentrations of angiogenetic markers [basic fibroblast growth factor (bFGF), fms related receptor tyrosine kinase(Flt)-1, phosphatidylinositol-glycan biosynthesis class F protein (PlGF), tyrosine-protein kinase(Tie)-2, vascular endothelial growth factor (VEGF)-C, VEGF-D], cytokines (IL-5, IL-7, IL-12/IL-23p40, IL-15, IL-16, IL-17A, TNF-β, VEGF-A), chemokines [Eotaxin, Eotaxin-3, interferon gamma-induced protein(IP)-10, macrophage-derived chemokine (MCP)-1, MCP-4, monocyte chemoattractant protein (MDC), macrophage inflammatory protein (MIP)-1α, MIP-1β, thymus and activation regulated chemokine (TARC)], proinflammatory cytokines [interferon(IFN)-γ, IL-2, IL-4, IL-6, IL-8, IL-10, TNF-α], and vascular injury markers [CRP, ICAM-1, soluble vascular adhesion molecule (VCAM)-1, serum amyloid A (SAA)] were analyzed using V-PLEX Neuroinflammation panel (Meso Scale Diagnostics, Rockville, MD, USA).
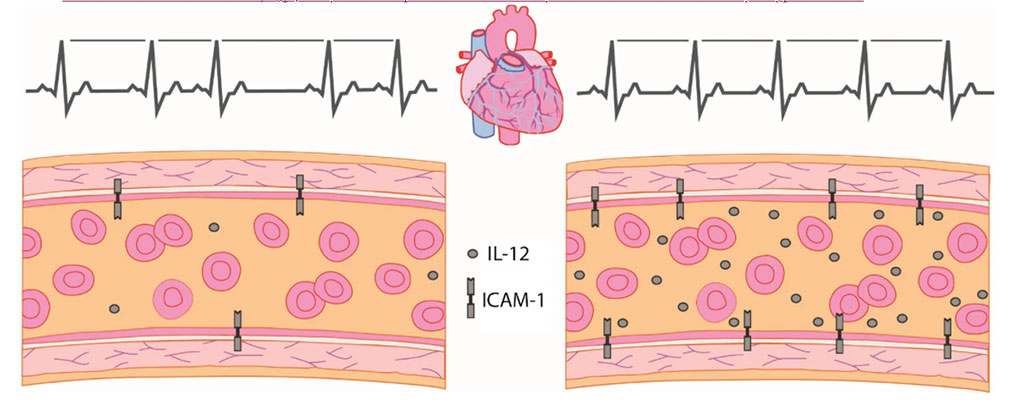
The investigators reported that out of 34 examined serum markers, they successfully measured six angiogenetic markers (bFGF, Flt-1, PIGF, Tie-2, VEGF-C, VEGF-D), six chemokines (Eotaxin, IP-10, MCP-1, MDC, MIP-1β, TARC), five cytokines (IL-7, IL-12/IL-23p40, IL-15, IL-16, VEGF-A), five proinflammatory markers (IL-6, IL-8, IL-10, IFN-γ, TNF-α), and four markers of vascular injury (CRP, sICAM1, sVCAM1, SAA), in more than 94% of the samples. Increased serum levels of IL-12/IL-23p40 and intercellular adhesion molecule (ICAM)-1 were associated with diminished heart rate variability measures. After all adjustments, the associations between IL-12/23p40, SDANN and VLF persisted. Additionally, serum levels of vascular endothelial growth factor (VEGF)-C were associated with response to standing.
The authors concluded that had found few but strong associations between neurocardiac function and serum markers, especially IL-12/IL-23p40, suggesting systemic changes in proinflammatory, endothelial, and lymphatic function, impacting overall cardiovascular function. The study was published on January 6 2022 in the journal Cardiovascular Diabetology.
Related Links:
Aalborg University Hospital
Meso Scale Diagnostics