Maternal Multiomic Changes Could Predict Onset of Labor
By LabMedica International staff writers
Posted on 18 May 2021
Currently, predictions of when labor will start are imprecise and based on gestational age and an average pregnancy length of 40 weeks, even though the onset of labor between week 37 and 42 of pregnancy is considered normal. Having a better idea of when labor may arrive could help with planning and managing medical concerns like fetal lung maturation.Posted on 18 May 2021
As pregnancy progresses toward labor, major transitions occur in fetomaternal immune, metabolic, and endocrine systems that culminate in birth. The comprehensive characterization of maternal biology that precedes labor is crucial to understanding these physiological transitions and identifying predictive biomarkers of delivery.
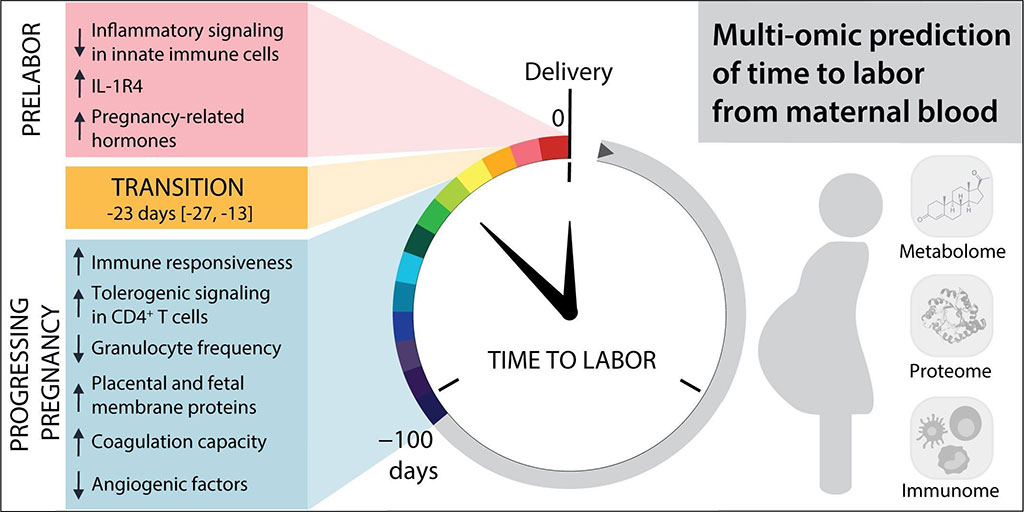
Image: Multiomic prediction of time to labor from biomarkers in maternal blood (Photo courtesy of STELZER ET AL.)
A large team of multidisciplinary scientists led by Stanford University School of Medicine (Palo Alto, CA, USA) followed more than 60 women toward the end of their pregnancies, collecting blood samples for metabolic, protein, and immune analysis. They collected a median of three blood samples from each participant within the 100 days preceding labor. Using untargeted mass spectrometry and an aptamer-based proteomic platform, the team tallied the levels of 3,529 metabolites and 1,317 proteins, while using a mass cytometry assay to gauge nearly 2,300 immune features over time.
The investigators pieces together a picture of the changes that occur in the two to four weeks prior to delivery. For instance, the levels of steroid hormones like progesterone and cortisol rose dramatically. At the same time, levels of factors involved in angiogenesis fell; a change they said could help weaken the connection between the uterus and the placenta, priming them for delivery.
Additional shifts affected the immune system. There was a rise in interleukin-1 receptor type 4 (IL-1R4) levels, which inhibits the inflammatory factor IL-33, suggesting that this change may tamp down inflammatory responses that might otherwise be triggered during labor. In addition, the increase in IL-1R4 levels could serve a labor-initiation signal. By feeding these changes into a model, the scientists developed a tool to predict when someone is about to go into labor. After training on their 53 cohort members, they tested their predictor on data from a further 10 women to find that it had high accuracy in predicting the time to labor. They further noted that the model could predict both preterm and term labor.
Virginia Winn, MD, an associate professor of obstetrics and gynecology and co-author of the study, said, “If we understand what's regulating labor, we might be able to do a better job of inducing labor.” The study was published on May 5, 2021 in the journal Science Translational Medicine.
Related Links:
Stanford University School of Medicine