Biomarker Protein Investigated in Juvenile Idiopathic Arthritis
By LabMedica International staff writers
Posted on 09 Mar 2021
Juvenile idiopathic arthritis (JIA) is the most common pediatric rheumatologic disease that may persist into adulthood and impact quality of life. The diagnosis is mainly based on clinical assessment rather than relying on laboratory testing.Posted on 09 Mar 2021
The disease course and prognosis of JIA may vary based on multiple factors such as presence of the biomarkers rheumatoid factor (RF) and cyclic citrullinated peptide (CCP) antibodies. RF-seropositive polyarticular JIA (PJIA RF+) has similar features as adult rheumatoid arthritis (RA) and may extend into adulthood. The biomarker 14–3-3η is highly sensitive and specific for RA in adults.
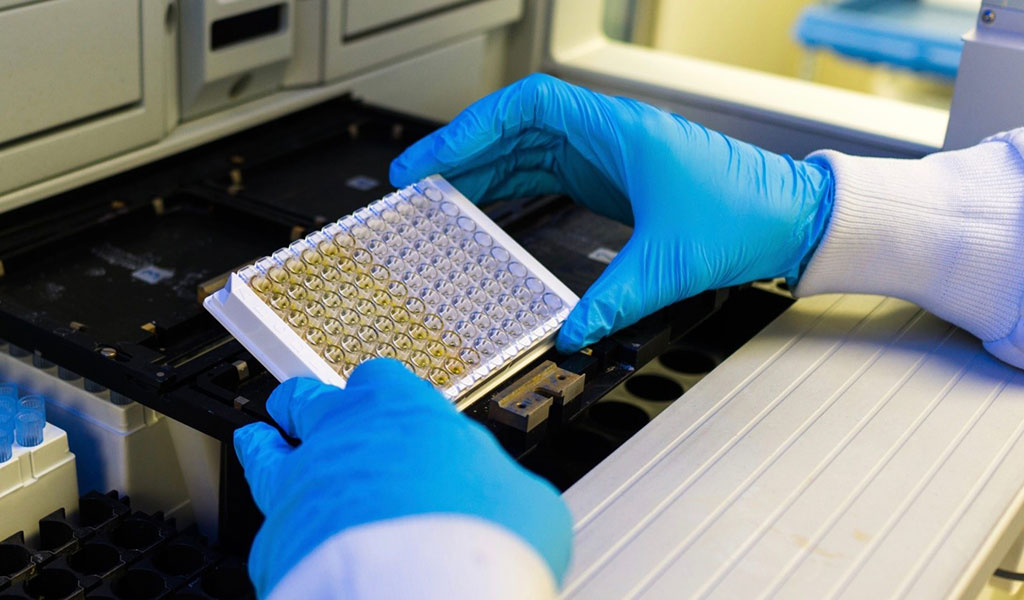
Image: An enzyme-linked immunosorbent assay (ELISA) measured serum 14–3-3η levels and evaluated in juvenile idiopathic arthritis (Photo courtesy of Quest Diagnostics).
Rheumatologists and their colleagues at the Children's Hospital of Los Angeles (Los Angeles, CA, USA) recruited 151 JIA patients who were categorized into five groups: polyarticular JIA RF+ (PJIA RF+; n = 39), PJIA RF- (n = 39), psoriatic arthritis (PsA; n = 19), enthesitis-related arthritis (ERA; n = 18), and oligoarticular JIA (OJIA [control group]; n = 36). Laboratory studies, including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), were obtained at the same time.
Specimens for CCP antibody, RF, antinuclear antibody (ANA), and HLA-B27 testing were also obtained. Samples for 14–3-3η were centrifuged and the serum was collected. Serum was stored in a freezer and sent to Quest Diagnostics Nichols Institute (San Juan Capistrano, CA, USA) overnight. 14–3-3η was measured via enzyme-linked immunosorbent assay (ELISA) at Quest Diagnostics. A 14–3-3η serum level of > 0.2 ng/mL was considered positive.
The team reported that elevated 14-3-3η levels were detected in 34/151 (23%) patients, and across all groups tested. Most patients with 14-3-3η had titers ≥4 times above the cutoff value. The majority (22, 65%) of 14-3-3η-positive patients were also positive for RF or CCP antibodies, 16 (47%) were positive for all three, and 12 (35%) were single-positive for 14-3-3η. The highest prevalence of 14-3-3η was in PJIA RF+ patients (49%), followed by OJIA (22%). Positivity for 14-3-3η was not significantly associated with disease activity or age at diagnosis.
The authors concluded that serum 14-3-3η can be detected in all forms of JIA tested, but appears to be most common in PJIA RF+. However, 14-3-3η does not appear to correlate with disease activity in JIA. The study was published on February 16, 2021 in the journal Pediatric Rheumatology.
Related Links:
Children's Hospital of Los Angeles
Quest Diagnostics














