Analysis of Nasal Polyps Suggests Mechanisms of Inflammation
By LabMedica International staff writers
Posted on 04 Sep 2018
Allergic inflammation can develop from persistent activation of type 2 immunity in the upper airway, resulting in chronic rhinosinusitis, which ranges in severity from rhinitis to severe nasal polyps.Posted on 04 Sep 2018
Basal cell hyperplasia is a hallmark of severe disease, but it is not known how these progenitor cells contribute to clinical presentation and barrier tissue dysfunction in humans. In an effort to elucidate molecular mechanisms of chronic inflammatory diseases, scientists have profiled the transcriptomes of human nasal polyps and nasal scrapings by single-cell RNA sequencing.
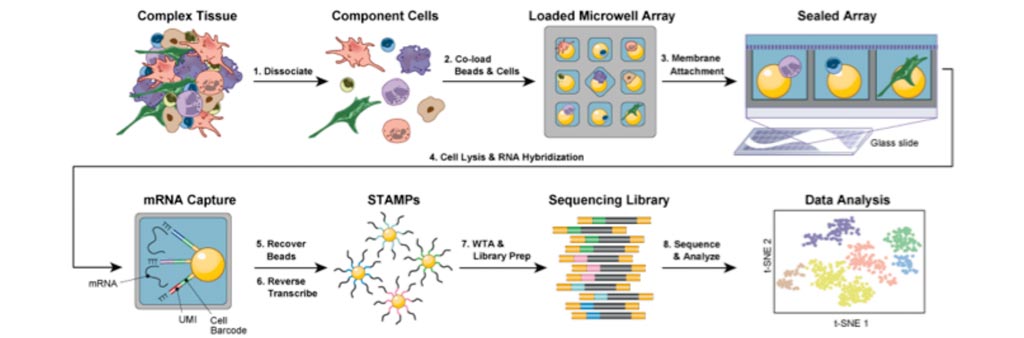
Image: Diagram of the Seq-Well low-cost platform for single-cell RNA sequencing (Photo courtesy of Shalek Lab).
Scientists at Brigham and Women's Hospital (Boston, MA, USA) and their colleagues performed single-cell RNA sequencing on more than 18,000 cells from 12 surgically removed nasal polyps spanning the disease spectrum. They used Seq-Well for massively parallel single-cell RNA sequencing, report transcriptomes for human respiratory epithelial, immune and stromal cell types and subsets from a type 2 inflammatory disease, and map key mediators. Seq-Well is a portable, low-cost platform for single-cell RNA sequencing designed to be compatible with low-input, clinical biopsies.
The investigators found that the diversity of epithelial cell types was reduced in the nasal polyps, which contained few glandular and ciliated cells and were enriched in basal cells. The latter appeared to be stuck in their ability to differentiate into other cell types. This reduction in cellular diversity might be explained by differences in gene expression the scientists found between polyp and non-polyp basal progenitor cells. In addition, they revealed that a transcriptional program that is activated by cytokines interleukin-4 (IL-4 ) and IL-13 is strongly induced in basal progenitor cells from polyps, suggesting a possible treatment with an antibody that blocks the shared IL-4/IL-13 receptor subunit.
The authors concluded that that reduced epithelial diversity stemming from functional shifts in basal cells is a key characteristic of type 2 immune-mediated barrier tissue dysfunction. Their results demonstrate that epithelial stem cells may contribute to the persistence of human disease by serving as repositories for allergic memories. The study was published on August 22, 2018, in the journal Nature.
Related Links:
Brigham and Women's Hospital













