Novel Blood Test Differentiates Celiac from Gluten Sensitivity
By LabMedica International staff writers
Posted on 24 Nov 2017
The measurement of circulating cytokines in blood plasma within six hours of eating gluten differentiated patients with celiac disease from those with non-celiac gluten sensitivity.Posted on 24 Nov 2017
Investigators found that a one-off oral gluten challenge caused an increase in interleukin (IL)-8, IL-10 and especially IL-2 in patients with celiac disease. Conversely, patients with non-celiac gluten sensitivity showed no measurable immune response to gluten, but did show a symptom response to Fermentable, Oligo-, Di-, Mono-saccharides and Polyols (FODMAPs), specifically fructans.
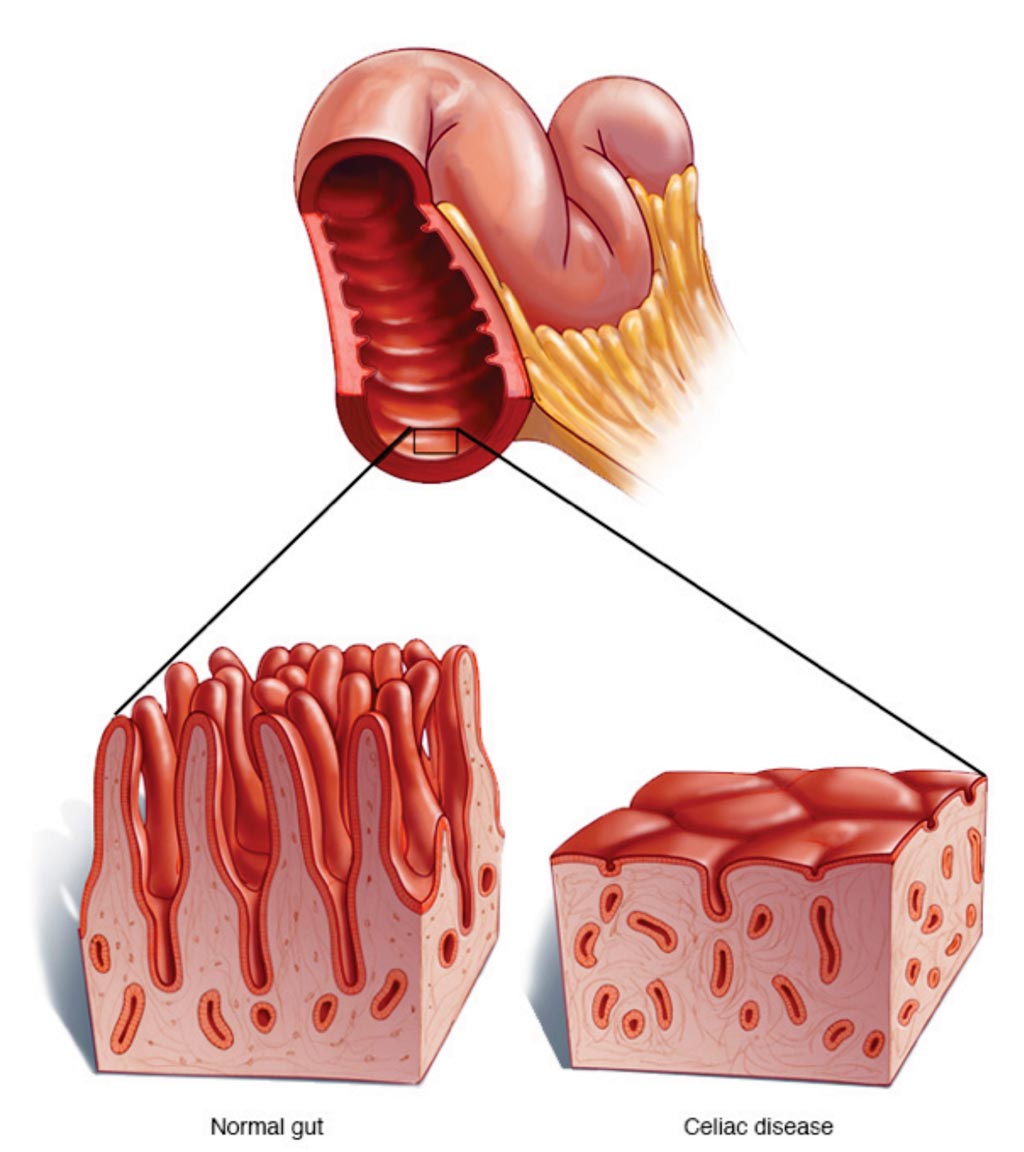
Image: A diagram comparing the small intestine in Celiac disease with damaged villi and a normal bowel (Photo courtesy of the Mayo Clinic).
Scientists at the University of Oslo (Norway) collaborating with those at ImmusanT (Cambridge, MA, USA) evaluated whether cytokine responses could distinguish between patients with celiac disease and non-celiac gluten sensitivity on a gluten-free diet. They evaluated IL-2, IL-8 and IL-10 plasma levels in 19 patients with celiac disease and 49 patients with non-celiac gluten sensitivity that underwent parallel food challenges. They drew blood samples before and 2, 4 and 6 hours after patients consumed breakfast bars containing gluten, FODMAP or placebo free of these ingredients.
Overall, the gluten-containing bars triggered mucosal changes in five of the patients with celiac disease, and induced a T-cell response in 12 of the 15 assessed. In contrast, the gluten-containing bars triggered no symptomatic response versus placebo in patients with non-celiac gluten sensitivity. Rather, these patients showed significantly higher irritable bowel syndrome symptom scores and bloating after consuming the FODMAP versus gluten bars. The team found that found that patients with celiac disease showed significant increases in IL-2 levels after consuming the gluten bars compared with non-celiac gluten sensitivity patients. At two hours the median elevations were 1.2-fold higher at four hours they were 10 times higher and at six hours they were 3.6 times higher.
Celiac patients also showed significantly higher increases in IL-8 and IL-10 relative to those with non-celiac gluten sensitivity at both four and six hours, but the median elevations were just between 1.2 to 1.8 times higher. Using optimized cutoffs, IL-2 identified celiac patients with 74% sensitivity and 98% specificity, while IL-8 performed with 42% sensitivity and 100% specificity, and IL-10 performed with 32% sensitivity and 100% specificity.
Robert P. Anderson, BMedSci, MB, ChB, PhD, FRACP, ImmusanT’s chief scientific officer, said, “It turns out that the people with celiac disease had an immune activation signature that we could measure in blood, and consistent with our previous study, this pointed to a T-cell effect, with gluten stimulating T-cells very quickly within 2 to 4 hours. But there was absolutely nothing that we could measure showing any form of immune activation in patients with non-celiac gluten sensitivity, which was surprising, because the immune activation in this condition is thought to be caused by the innate immune system releasing markers like IL-8.” The study was presented at the United European Gastroenterology Week 2017 held October 28 – November 1, in Barcelona, Spain.
Related Links:
University of Oslo
ImmusanT