Hematological Neoplasm Cytogenetics Profiled With Optical Genome Mapping
Posted on 25 Oct 2022
The current standard-of-care cytogenetic techniques for the analysis of hematological malignancies include karyotyping, fluorescence in situ hybridization, and chromosomal microarray analysis (CMA), which are labor intensive and time and cost prohibitive, and they often do not reveal the genetic complexity of the tumor, demonstrating the need for alternative technology for better characterization of these tumors.
Optical genome mapping (OGM) has emerged as a next-generation cytogenomic technology that can detect all classes of SVs at a higher resolution than the standard-of-care (SOC) techniques. Recently, the technology has gained enormous traction and has been evaluated in several settings, including prenatal settings, postnatal settings, hematological neoplasms, and solid tumors, demonstrating 100% clinical concordance with traditional cytogenetic analysis.

Medical Scientists at the Medical College of Georgia (Augusta, GA, USA) performed a retrospective validation study included 92 analyses (including replicates), representing 69 unique and well-characterized samples that were received in their clinical laboratory for cytogenetic analysis with karyotyping and/or FISH testing. These were composed of 59 hematological neoplasms that included 18 adult acute myeloid leukemia (AML), 15 chronic lymphocytic leukemia (CLL), 12 myelodysplastic syndrome (MDS), six plasma cell myeloma, three lymphoma, three myeloproliferative disorders/myeloproliferative neoplasms, and two chronic myeloid leukemia. In addition, 10 morphologically normal and cytogenetically negative samples were also analyzed to evaluate true-negative/false-positive rates and calculate performance metrics.
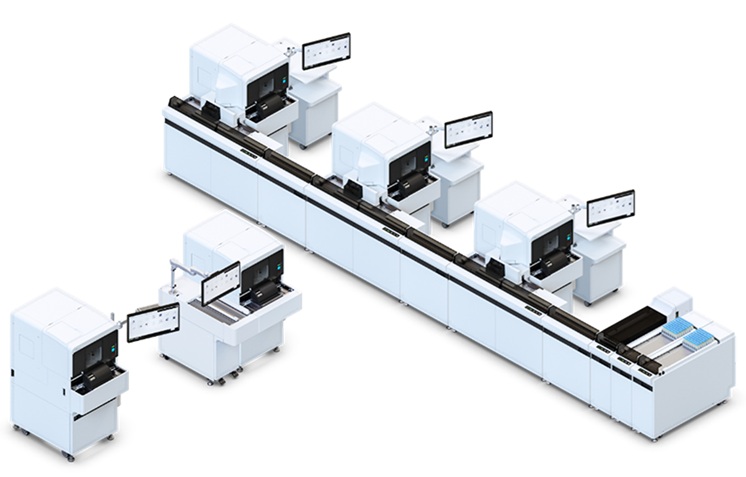
Ultra-high-molecular-weight DNA was isolated, labeled, and processed for analysis on the Bionano Genomics Saphyr platform (Bionano Genomics Inc., San Diego, CA, USA). A frozen bone marrow aspirate aliquot (650 μL) was thawed, and cells were counted using HemoCue (HemoCue Holding AB, Ängelholm, Sweden). The DNA backbone was stained blue using DNA stain and quantified using Qubit high-sensitivity double-stranded DNA assay kits. Labeled DNA was loaded onto flow cells of Saphyr chips for optical imaging. The fluorescently labeled DNA molecules were imaged on the Saphyr instrument after the labeled DNA molecules were electrophoretically linearized in the nanochannel arrays.
The team reported that all 69 samples passed the quality control metrics, and the 59 hematological neoplasm samples achieved an average N50 (>150 kb) of 303 kb (±35), map rate of 87.5% (±7.5%), label density of 15.8/100 kb (±1.0), and average coverage of 391× (±89). In total, 86,306 SVs were identified in the 59 samples, with an average of approximately 1,462 SVs per sample. OGM was concordant in identifying 162 of 164 variants, which were reported with current SOC methods. OGM detected 59 of 60 aneuploidies, whereas one mosaic loss of chromosome Y (in a complex case of CLL) was not detected with OGM.
Of the 45 cases classified as simple, 35 had at least one clinically reported genetic aberration, whereas 10 were negative with both karyotyping and/or FISH testing. In the 35 cases with reported aberrations, OGM detected all of the previously reported variants and corrected the previously incorrect interpretations due to low resolution of karyotyping in two cases. The translocation, interstitial deletion, and duplication were detected consistently from 25% to 5% allele fraction.
The authors concluded that their study showed a 98.7% sensitivity and a 100% specificity for detecting SVs previously reported with a combination of SOC methods. The increased clinical utility of OGM in hematological malignancies has been established by multiple reports where 100% concordance was reported with multiple SOC methods. The study was published on October 17, 2022 in the Journal of Molecular Diagnostics.
Related Links:
Medical College of Georgia
Bionano Genomics
HemoCue Holding AB