Cardiac Biomarkers Investigated in Acquired Refractory Thrombocytopenic Purpura Patients
Posted on 21 Jun 2022
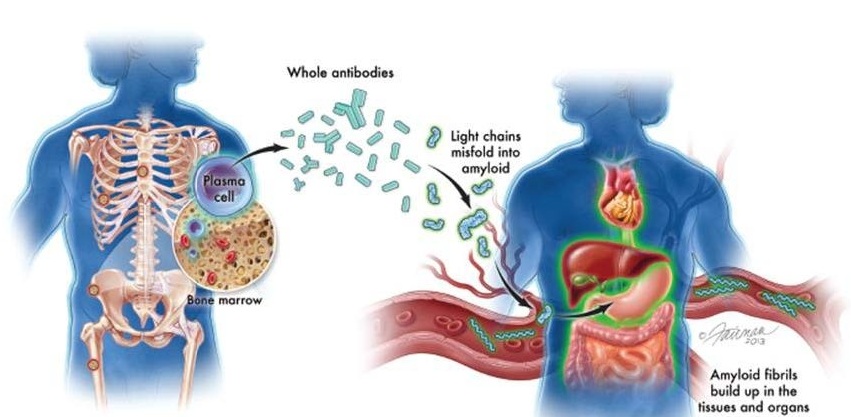
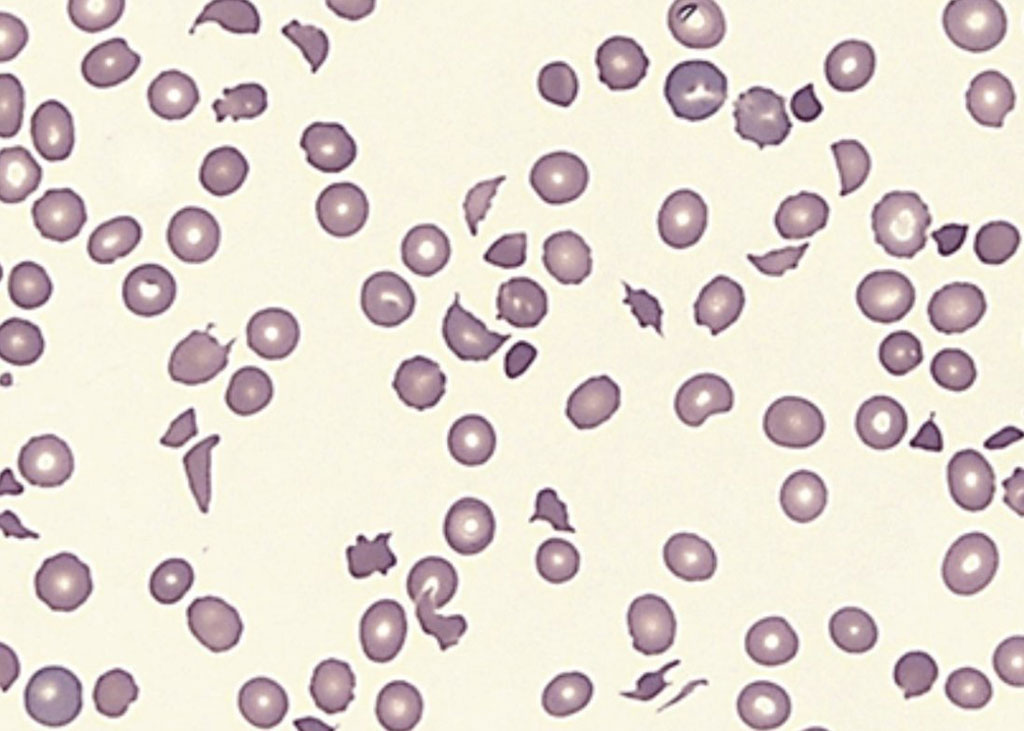
Thrombotic thrombocytopenic purpura (TTP) is a rare disorder that causes blood clots (thrombi) to form in small blood vessels throughout the body. These clots can cause serious medical problems if they block vessels and restrict blood flow to organs such as the brain, kidneys, and heart.
Cardiovascular complications of TTP were first reported in a patient whose postmortem autopsy revealed diffusive thrombosis of terminal arteries and capillaries. Subsequently studies demonstrated that acute myocardial infarction and cardiac arrest are the leading causes of death in patients with TTP.
Hematologists at The First Affiliated Hospital of Soochow University (Suzhou, China) enrolled patients in a study who were diagnosed with refractory TTP from 2013 through 2020. The inclusion criteria were: (1) fever, hematuria, neurological involvement, or other TTP manifestations; (2) acute peripheral thrombocytopenia (<100 × 109/L), but no other identifiable cause; (3) decreased ADAMTS13 activity level (<10%); (4) positive anti-ADAMTS13 autoantibodies; (5) failure of platelet response after 4–7 days of therapeutic plasma exchange (TPE); (6) a clinical deterioration in a patient receiving standard therapy.
Baseline characteristics, including demographic information, clinical manifestations, and previous medical history, were collected from electronic health records (EHR). Laboratory information, including aspartate aminotransferase (AST), alanine aminotransferase (ALT), high-sensitivity cardiac troponin T (hs-cTnT), and N-terminal probrain natriuretic peptide (NT-proBNP), were collected and recorded on admission and on the next day after last TPE treatment, respectively.
The investigators reported of the 78 patients with refractory TTP that were included in the study, 21 patients died during hospitalization with a mortality rate of 26.9% (21/78) and a median time to in-hospital death of 8.05 days. On-admission serum hs-cTnT (66.15 [14–410] versus 29.31 [12.5–90.04] pg/mL), NT-proBNP (1401 [439.5–4,490] versus 1,200.6 [235.18–2,756] pg/mL), and the ASTL: ALT ratios (AAR: 1.97 [1.41–2.86] versus 1.56 [1.07–2.21]) were significantly increased in the patients who died in hospital compared to those who survived. Multivariate analysis showed that AAR after TPE was associated with overall mortality (OR: 4.45). The areas under the receiver operator characteristic curve (AUC) of AAR, hs-cTnT, and NT-proBNP for the association with mortality were 0.814, 0.840, and 0.829, respectively.
The authors concluded that their results suggest that increased post-TPE cardiac markers were associated with death in TTP. AAR is a strong predictor for mortality and may be used for risk stratification in future TTP management. The study was published on June 11, 2022 in the Journal of Clinical Laboratory Analysis.
Related Links:
The First Affiliated Hospital of Soochow University