Cord Blood and Matched Related Donor Transplantation Compared in Acute Myeloid Leukemia
By LabMedica International staff writers
Posted on 19 Jan 2022
The prognosis of primary refractory and relapsed acute myeloid leukemia is poor, with a five-year overall survival of less than 10%. Allogeneic hematopoietic stem cell transplantation (HSCT) is the only curative treatment option for these patients.Posted on 19 Jan 2022
Cord blood transplantation (CBT) is an alternative donor transplantation method and has the advantages of rapid availability and the possibility of inducing a more potent graft-versus-leukemia effect, leading to a lower relapse rate for patients with non-remission relapse and refractory acute myeloid leukemia (R/R AML).
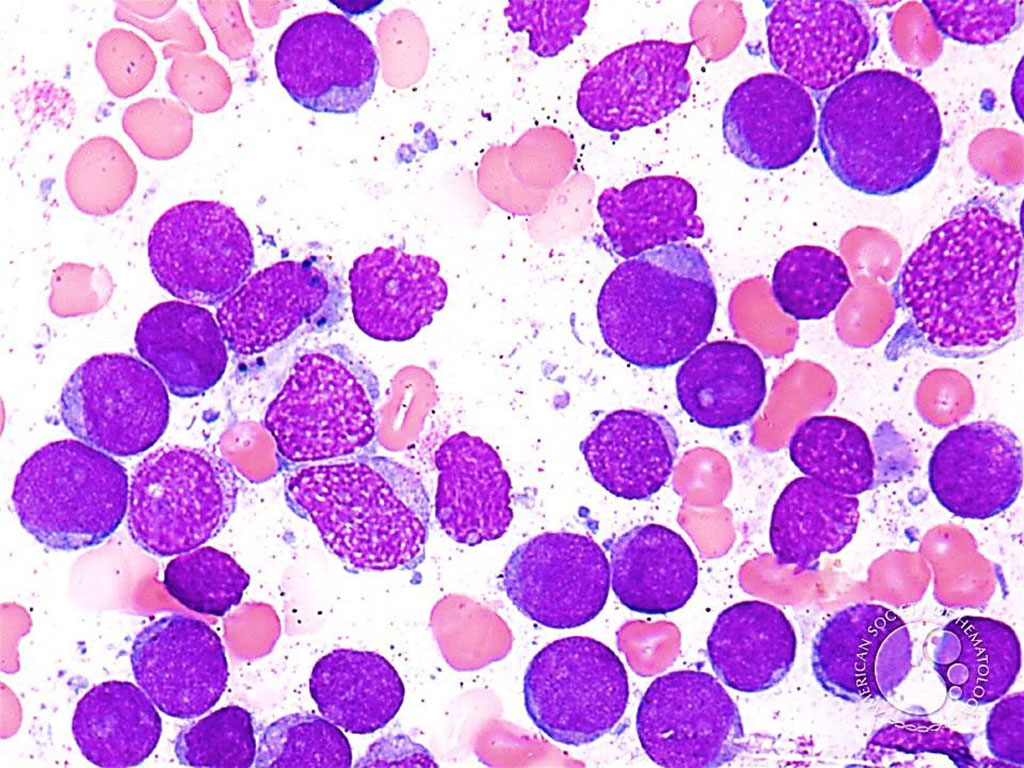
Image: Bone marrow aspirate from a patient with Acute Myeloid Leukemia: Blasts are the predominant population and have a high nuclear to cytoplasmic ratio and generally lack granules. (Photo courtesy of Professor Peter G. Maslak, MD)
A large team of Hematologists at the Graduate School of Medicine Kyoto University (Kyoto, Japan) and their colleagues investigated the impact of CBT, compared to human leukocyte antigen-matched related donor transplantation (MRDT). The study included 2,451 adult patients with non-remission R/R AML who received CBT (1,738 patients) or MRDT (713 patients) between January 2009 and December 2018. The median age was 55 years (interquartile range, 43–63 years), with 1,484 patients (61%) being male. Karyotype risk, was estimated as 190 (8.2%), 1,352 (59%), and 768 (33%) patients had favorable, intermediate, and poor karyotypes, respectively.
There were 1,499 (61%) patients with primary induction failures and 952 (39%) with relapses. Among these patients, 1,576 (65%) had blasts in the peripheral blood. The myeloablative conditioning regimen (MAC) and reduced-intensity conditioning regimen were defined as previously described. HLA match was defined as the same serologically identified HLA-A, HLA-B, and HLA-DRB1 between the donor and recipient. Comparisons were made by examining the 5-year progression-free survival (PFS) rates of these Japanese patients.
The investigators reported that the primary endpoint, the 5-year PFS, was 22.2% (95% CI: 20.1–24.3%) in the CBT group and 19.9% (95% CI: 16.8–23.1%) in the MRDT group. The adjusted hazard ratio (HR) was 0.83 (95% CI: 0.69–1.00); this was due to a more pronounced decrease in the relapse rate (HR: 0.78, 95% CI: 0.69–0.89) than an increase in the non-relapse mortality (NRM: 1.42, 1.15–1.76). The CBT group had more patients with infection-related death and fewer patients with graft-versus-host disease (GVHD)-related deaths and death due to primary diseases.
Yoshimitsu Shimomura, MD, a Hematologist and the lead author of the study, said, “We believe CBT would be a great treatment option for R/R AML patients in non-remission given the circumstances. However, there are currently limited data for how this subset of patients would respond to CBT. Before comparing PFS rates, we performed propensity score matching. This took into account factors such as patient age, sex, years of treatment, and others to ensure all comparisons were as fair as possible and no biases were introduced. CBT compared with MDRT that had a more pronounced decrease in relapse rate than increase in NRM.”
The authors concluded that their data support CBT as a potential superior alternative to MRDT for patient prognosis and thus provide evidence which may influence clinical guidelines on R/R AML treatment. Future studies will investigate if genetic factors play any roles in patients’ responses to these two transplantation methods. Additionally, patient quality of life will be considered to optimize therapeutic development for this deadly disease. The study was originally published on November 21, 2021 in the journal Leukemia.
Related Links:
Graduate School of Medicine Kyoto University