Fecal Calprotectin Predicts Therapy Outcome in Ulcerative Colitis Patients
By LabMedica International staff writers
Posted on 24 Aug 2021
Ulcerative colitis (UC) is a chronic intestinal disorder of unknown etiology and characterized by a relapsing and remitting course. The diagnosis and assessment of the disease activity has been based on clinical symptoms, laboratory measurements, findings of endoscopy and pathological examinations.Posted on 24 Aug 2021
The development of a non-invasive and simple biomarker for evaluating the disease activity is considered necessary for the clinical management of UC. Calprotectin is a complex of mammalian proteins found in the cytosol of human neutrophils, monocytes and macrophages. Granulocyte and monocyte adsorptive apheresis (GMA) is widely used as a remission induction therapy for active UC patients.
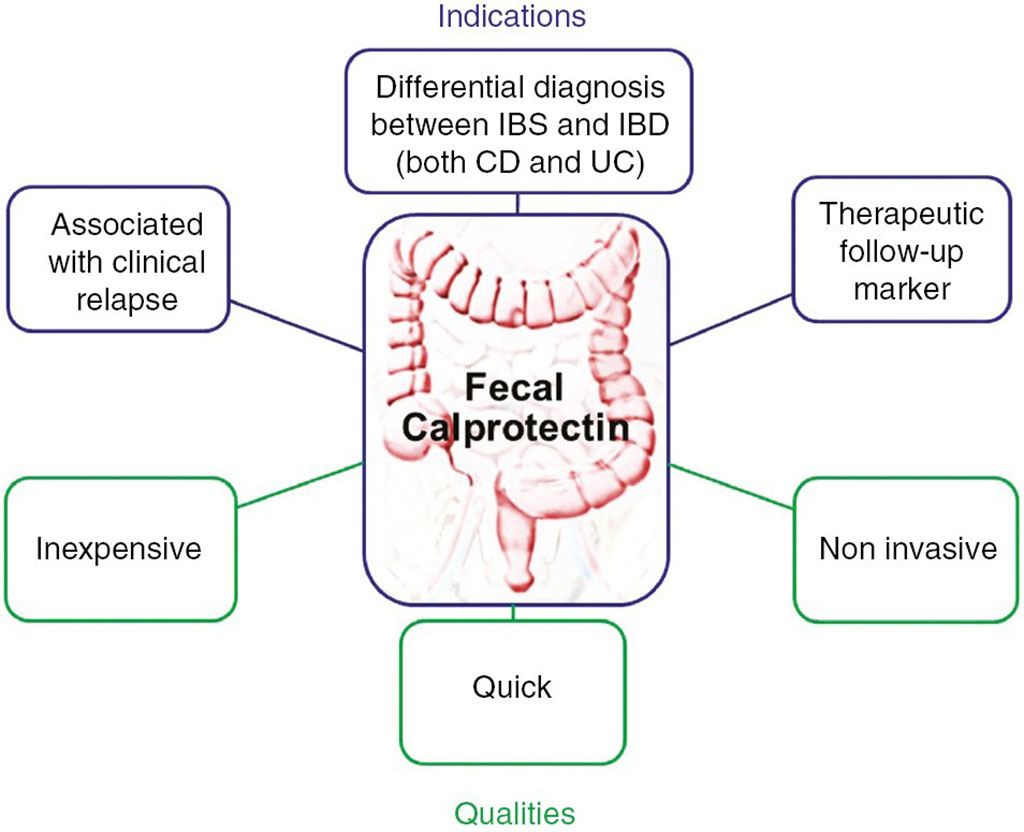
Image: Schematic representation of calprotectin indications in clinical practices and main advantages (Photo courtesy of Hôpital Beaujon)
A large team of Gastroenterologists at the (Asahikawa Medical University, Asahikawa, Japan) and their colleagues conducted a multicenter prospective observation study of patients who received 10 sessions of GMA, twice a week, for five consecutive weeks. A total 36 patients with active UC were enrolled in the study. Fecal calprotectin was measured at entry, one week, two weeks, at the end of GMA and on the day of endoscopy within 24 weeks after GMA.
The patients’ stool samples were homogenized by mixing with a predefined extraction buffer volume. After centrifugation, the supernatants were subjected to a fluorescence enzyme immunoassay using EliA Calprotectin 2 (Thermo Fisher Scientific, Tokyo, Japan). Laboratory values, including the white blood cell (WBC) count and C- reactive protein (CRP) level were also measured at the same time points as FC measurement: at entry, one and two weeks and at the end of GMA and on the day when endoscopy was performed within 24 weeks after GMA. The team analyzed the relationships between the clinical outcome (clinical remission [CR] and endoscopic remission [ER]) and the change in FC concentration.
The investigators reported that the overall CR and ER rates were 50.0% and 19.2%, respectively. After GMA, the median FC concentration in patients with ER was significantly lower than that in patients without ER (469 mg/kg versus 3,107 mg/kg). When the cut-off value of FC concentration was set at 1,150 mg/kg for assessing ER after GMA, the sensitivity and specificity were 0.8 and 0.81, respectively. The FC concentration had significantly decreased by one week. An ROC analysis demonstrated that the reduction rate of FC (ΔFC) at one week was the most accurate predictor of CR at the end of GMA (AUC = 0.852). When the cut-off value of ΔFC was set at ≤ 40% at one week for predicting CR at the end of GMA, the sensitivity and specificity were 76.9% and 84.6%, respectively.
The authors concluded that they had evaluated the utility of FC as a biomarker for assessing ER after GMA and predicting CR in the early phase during GMA in patients with active UC. The findings will benefit patients with active UC by allowing them to avoid unnecessary invasive procedures and will help establish new strategies for GMA. The study was published on August 6, 2021 in the journal BMC Gastroenterology.
Related Links:
Asahikawa Medical University
Thermo Fisher Scientific














