Coagulation and Fibrinolysis Assessed in Splenic Injury Patients
By LabMedica International staff writers
Posted on 19 May 2021
The most frequently injured solid organ following blunt abdominal trauma is the spleen. Splenectomy was a standard surgical procedure for splenic injury until the mid‐20th century. However, thrombotic and infectious complications following splenectomy were demonstrated by many studies.Posted on 19 May 2021
Thrombocytosis, alterations of coagulation and fibrinolysis contribute to hypercoagulability and thromboembolism. Platelet (PLT) count, fibrinogen (FIB), D‐dimers (D‐D), fibrinogen/fibrin degradation products (FDP), antithrombin III (AT III) are key markers of coagulation and fibrinolytic activity. Prothrombin time (PT), activated partial thromboplastin time (APTT), and thrombin time (TT) are used for routine coagulation testing.
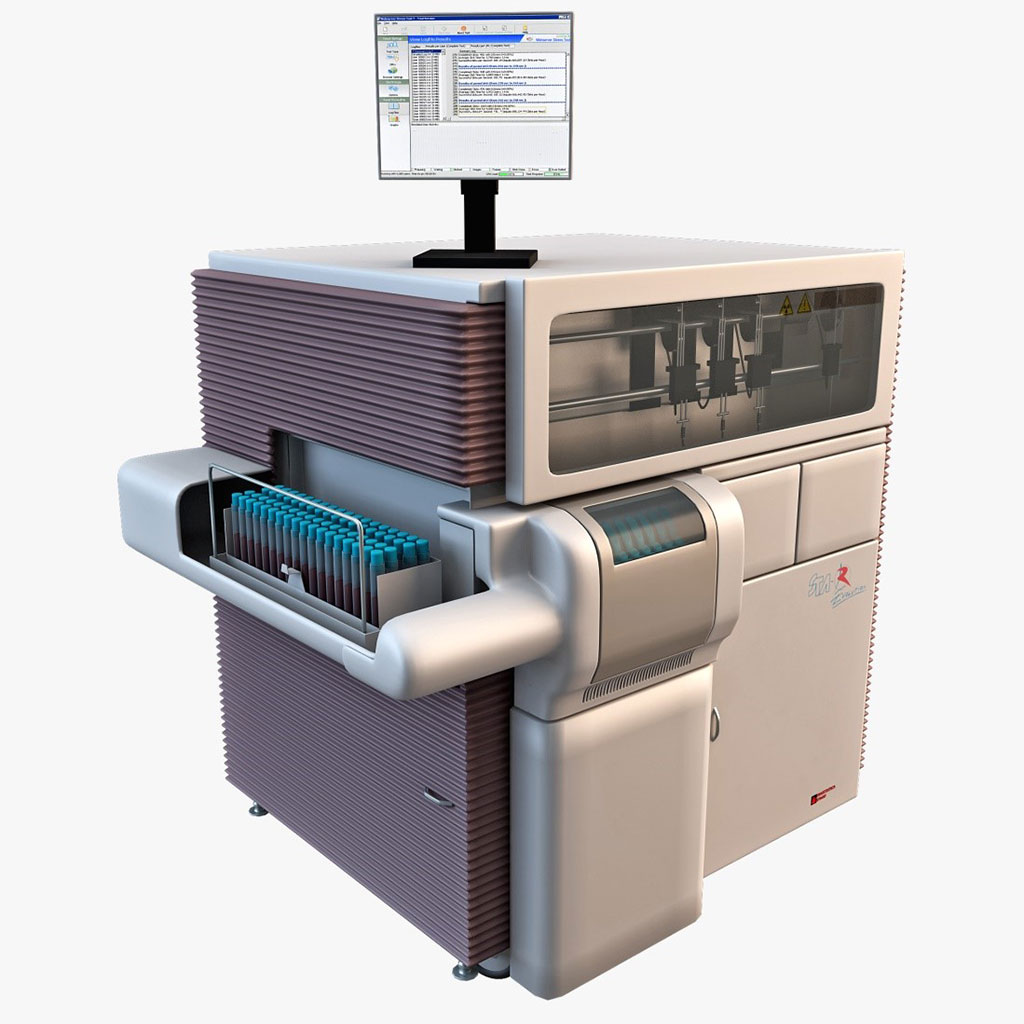
Image: The Star Evolution coagulation analyzer (Photo courtesy of Diagnostica Stago)
Emergency Medicine Specialist at the University of Science and Technology of China (Hefei, China) included in a study 38 blunt splenic injury (BSI). Splenic artery embolization (SAE) was performed if the splenic injury was classed as grade III or greater and had no requirement of immediate surgery.
Blood samples were collected in tubes containing EDTA for PLT count and Hb, hematocrit (Hct) determinations, which were determined using Sysmex XE‐5000 automated hematology analyzer (Sysmex, Kobe, Japan). Samples were collected in tubes containing 3.2% sodium citrate and then centrifuged at 2,000 rpm for 20 minutes to obtain plasma, which was used for determining coagulation and fibrinolysis parameters. FIB, D‐D, FDP, AT III, PT, APTT, and TT were measured on the STA‐R Evolution automated coagulation analyzer with identical commercial kit (Diagnostica Stago, Asnieres, France).
The medical team reported that the technical success rate of SAE and the splenic salvage rate were 100%. There was no mortality. Compared with pre‐SAE values, the levels of PLT, FIB, D‐D, and FDP increased significantly at three days and seven days after SAE. However, AT III, PT, APTT, TT, Hb, and Hct showed no statistically significant difference at one day, three days, and seven days after SAE.
The authors concluded that they had demonstrated that PLT significantly increased and activation of coagulation and fibrinolysis took place in BSI patients undergoing SAE. These alterations might have contributed to the increased risk of thrombotic complications, especially three days and seven days after SAE. Despite SAE as a critical treatment is used extensively in BSI patients and has increased the success rate of NOM, thromboembolism following SAE should be considered and thrombotic prophylaxis should be recommended. The study was published on May 6, 2021 in the Journal of Clinical Laboratory Analysis.
Related Links:
University of Science and Technology of China
Sysmex
Diagnostica Stago