Coagulation Dysfunction and Infection Evaluated in Patients with AECOPD
By LabMedica International staff writers
Posted on 14 Apr 2021
Chronic obstructive pulmonary disease (COPD) is one of the common chronic airway obstructive diseases, characterized by persistent respiratory symptoms and airflow limitation. In acute exacerbation stage (AECOPD), patients developed respiratory failure often have circulatory and coagulation dysfunction, which was considered the cause of thrombosis events in the patients.Posted on 14 Apr 2021
Although the inflammation in the early stage of COPD only involves the trachea and lung, hypoxia and further acute inflammation are systemic. In acute exacerbation stage, patients developed respiratory failure often have circulatory and coagulation dysfunction, which was considered the cause of thrombosis events in the patients. The coagulation abnormality could cause pulmonary embolism, myocardial infarction, cerebral infarction, and other thrombosis events in COPD patients.
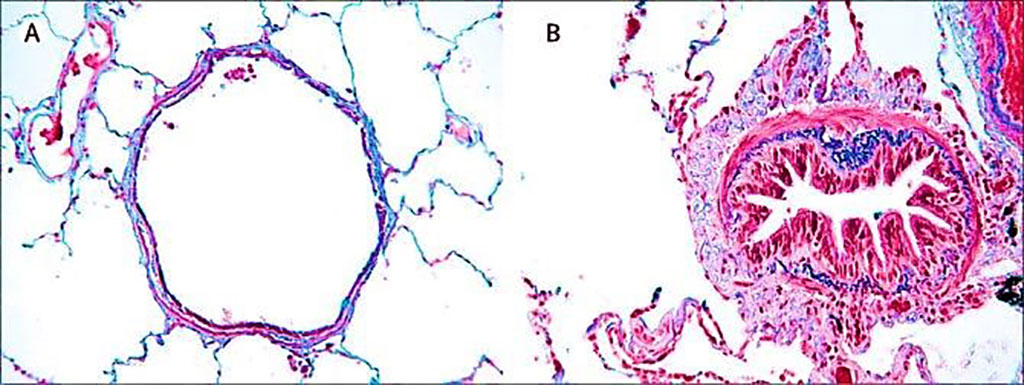
Image: Histology comparison of airway features in (A) a healthy individual and (B) in a patient with chronic obstructive pulmonary disease where airways are narrowed by infiltration of inflammatory cells, mucosal hyperplasia, and deposition of connective tissue in the peribronchiolar space (Photo courtesy of University of Leuven)
Respiratory and Critical Care Medicine Scientists from the Anhui Medical University (Hefei, China) performed a retrospective clinical study to investigate the factors correlated to abnormal coagulation status in COPD from November 2016 to November 2019. A total of 135 AECOPD, 44 stable stage COPD patients, and 135 healthy controls were enrolled in this study. The coagulation parameters, blood gas indexes and blood routine examination results were collected and analyzed.
The scientists reported that white blood count (WBC), neutrophil count, neutrophil percentage (N%), platelet (PLT), prothrombin time (PT), international normalized ratio (INR), fibrinogen (FIB), and activated partial thromboplastin time (APTT) increased, plasma thrombin time (TT) decreased in AECOPD group compared with the control group. In AECOPD group, PT, APTT, and FIB were positively correlated with neutrophils and C‐reaction protein levels. PT was positively correlated with partial pressure of carbon dioxide (PCO2) and negatively with pH. Thrombosis was observed in five acute exacerbation and three stable stage COPD patients. In 38 patients with abnormal blood gas analysis indexes, PT level was negatively correlated with pH, positively correlated with arterial partial pressure of carbon dioxide (PaCO2) levels indicating abnormal coagulation status was correlated to hypercapnia and acidosis.
The authors concluded that their study revealed that coagulation dysfunction existed in AECOPD patients. The abnormal coagulation was correlated to infection and hypercapnia and might be the main cause of thrombosis in the patients. The study was published on March 25, 2021 in the Journal of Clinical Laboratory Analysis.
Related Links:
Anhui Medical University









 (3) (1).png)




