New Technology Rapidly Diagnoses Sickle Cell Disease
By LabMedica International staff writers
Posted on 29 Oct 2020
Sickle cell disease (SCD) is a group of blood disorders typically inherited from a person's parents. The most common type is known as sickle cell anemia (SCA). It results in an abnormality in the oxygen-carrying protein hemoglobin found in red blood cells.Posted on 29 Oct 2020
Sickle cell disease occurs when a person inherits two abnormal copies of the β-globin gene that makes hemoglobin, one from each parent. This gene occurs in chromosome 11. Several subtypes exist, depending on the exact mutation in each hemoglobin gene. An attack can be set off by temperature changes, stress, dehydration, and high altitude.
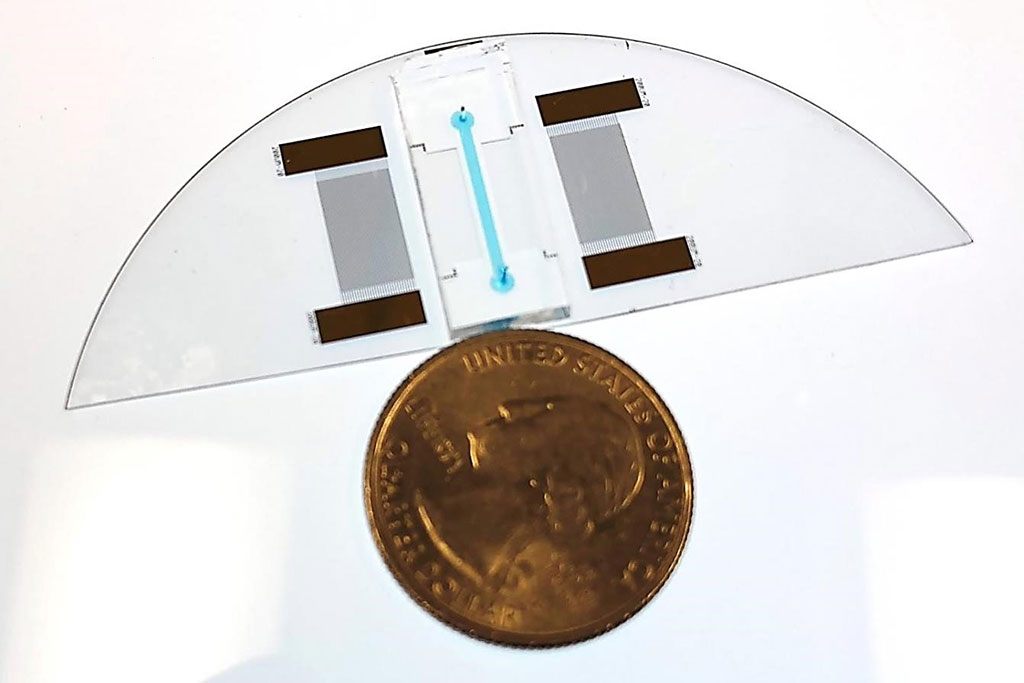
Image: An Acousto Thermal Shift Assay `lab-on-a-chip` device shown next to a US quarter for size comparison. The device can diagnose sickle cell anemia (Photo courtesy of CU Boulder College of Engineering and Applied Science).
Molecular, Cellular and Developmental Biologists at the University of Colorado, (Boulder, CO, USA) have developed a new way to diagnose diseases of the blood like sickle cell disease with sensitivity and precision and in only one minute. Their technology is smaller than a quarter and requires only a small droplet of blood to assess protein interactions, dysfunction or mutations. The team used Thermal Shift Assays (TSAs) to assess protein stability under varying conditions. Such tests took about a day to run. Now, with the new technology, an Acousto Thermal Shift Assay (ATSA), they can do the same but faster and with greater sensitivity.
Proteins have a specific solubility at a specific temperature. The solubility changes when one protein bonds to another, or when the protein is mutated, by measuring solubility at different temperatures, scientists can tell whether the protein has been mutating. The ATSA utilizes high-amplitude sound waves, or ultrasound, to heat a protein sample. The tool then measures data continuously, recording how much of the protein has dissolved at every fraction of change in degrees Celsius. The ATSA requires only a power source, a microscope and a camera as simple as the one on a smartphone. Because the protein is concentrated, there is also no need to apply a florescent dye as is sometimes required to highlight protein changes in a traditional TSA.
Yonghui Ding, PhD, a post-doctoral fellow and the first author of the study, said, “The method is seven to 34 times more sensitive. The ATSA can distinguish the sickle cell protein from normal protein, while the traditional TSA method cannot.” The study was published on October 15, 2020 in the journal Small.
Related Links:
University of Colorado














