Molecule in Lymphatic System Implicated in Autoimmune Diseases
By LabMedica International staff writers
Posted on 02 Apr 2020
A healthy immune system defends the body against diseases and infection. When someone has an autoimmune disease, the immune system malfunctions and the body mistakenly attacks healthy cells, tissues and organs. Rheumatoid arthritis, lupus and scleroderma are examples of autoimmune diseases.Posted on 02 Apr 2020
Non-hematopoietic stromal cells in lymph nodes such as fibroblastic reticular cells (FRCs) can support the survival of plasmablasts and plasma cells together which are antibody-forming cells (AFCs). However, a regulatory function for the stromal compartment in AFC accumulation has not been fully studied.
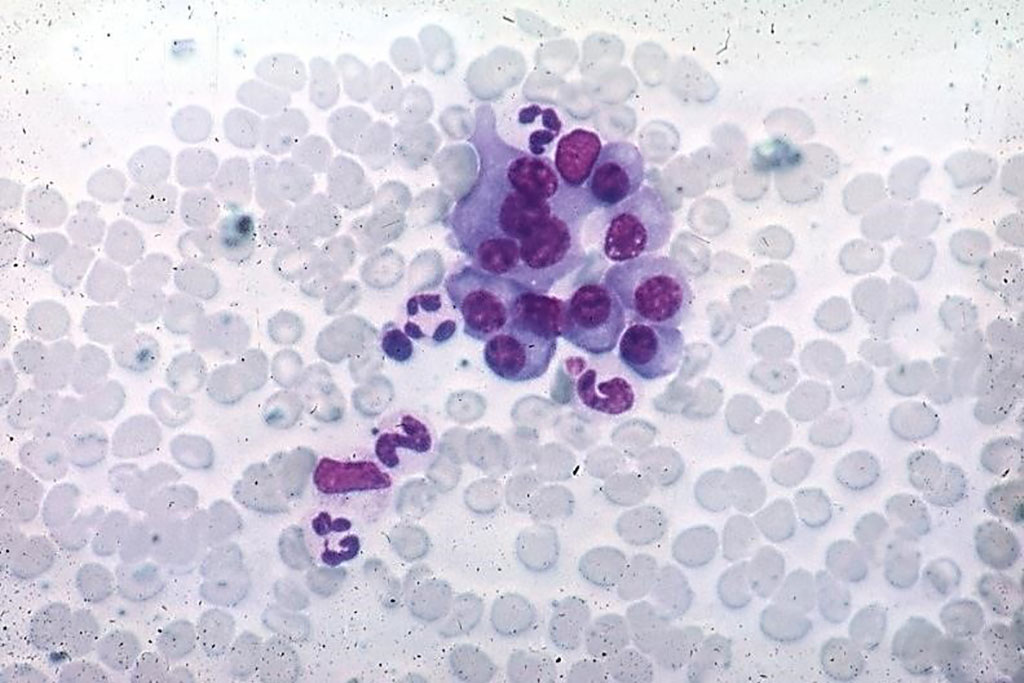
Image: Photomicrograph of normal plasma cells from a bone marrow aspirate (Photo courtesy of Peter Anderson).
Scientists at the Hospital for Special Surgery (New York, NY, USA) and their colleagues have shown that chemokine ligand 2 (CCL2)–expressing stromal cells limit AFC survival. FRCs express high levels of CCL2 in vessel-rich areas of the T cell zone and the medulla, where AFCs are located. FRC CCL2 is up-regulated during AFC accumulation, and the team used lymph node transplantation to show that CCL2 deficiency in BP3+ FRCs and lymphatic endothelial cells increases AFC survival without affecting B or germinal center cell numbers.
Monocytes are key expressers of the CCL2 receptor CCR2, as monocyte depletion and transfer late in AFC responses increases and decreases AFC accumulation, respectively. Monocytes express reactive oxygen species (ROS) in an NADPH oxidase 2 (NOX2)–dependent manner, and NOX2-deficient monocytes fail to reduce AFC numbers. Stromal CCL2 modulates both monocyte accumulation and ROS production, and is regulated, in part, by manipulations that modulate vascular permeability.
Theresa T. Lu, MD, PhD, a Professor of Microbiology and Immunology, and senior author of the study, said, “As the immune system is so central to how well our bodies function and often acts in similar ways in a number of different settings, what we are learning about manipulating fibroblasts can also help the biomedical community better understand how to treat related processes, such as healing after a musculoskeletal injury, fighting cancer and fighting infections. For example, medications used in adults and children with different forms of autoimmune inflammatory arthritis or lupus are being examined in the setting of coronavirus infections.” The study was published on March 20, 2020 in the journal Science Immunology.
Related Links:
Hospital for Special Surgery










 (3) (1).png)