Hypercoagulability Evaluated in New‐Onset Systemic Lupus Erythematosus Patients
By LabMedica International staff writers
Posted on 30 Dec 2019
Systemic lupus erythematosus (SLE) is an autoimmune inflammatory disease that involves T cell, B cell, and dendritic cell dysfunction, as well as antinuclear autoantibody production. Several clinical and scientific studies of SLE indicate an increased risk of thrombosis in these cases.Posted on 30 Dec 2019
The traditional parameters for screening coagulopathy include prothrombin time (PT) and activated partial thromboplastin time (aPTT). The thromboelastography (TEG) procedure facilitates the functional evaluation of the coagulation cascade, from clot formation to clot lysis, and provides data on the entire coagulation system.
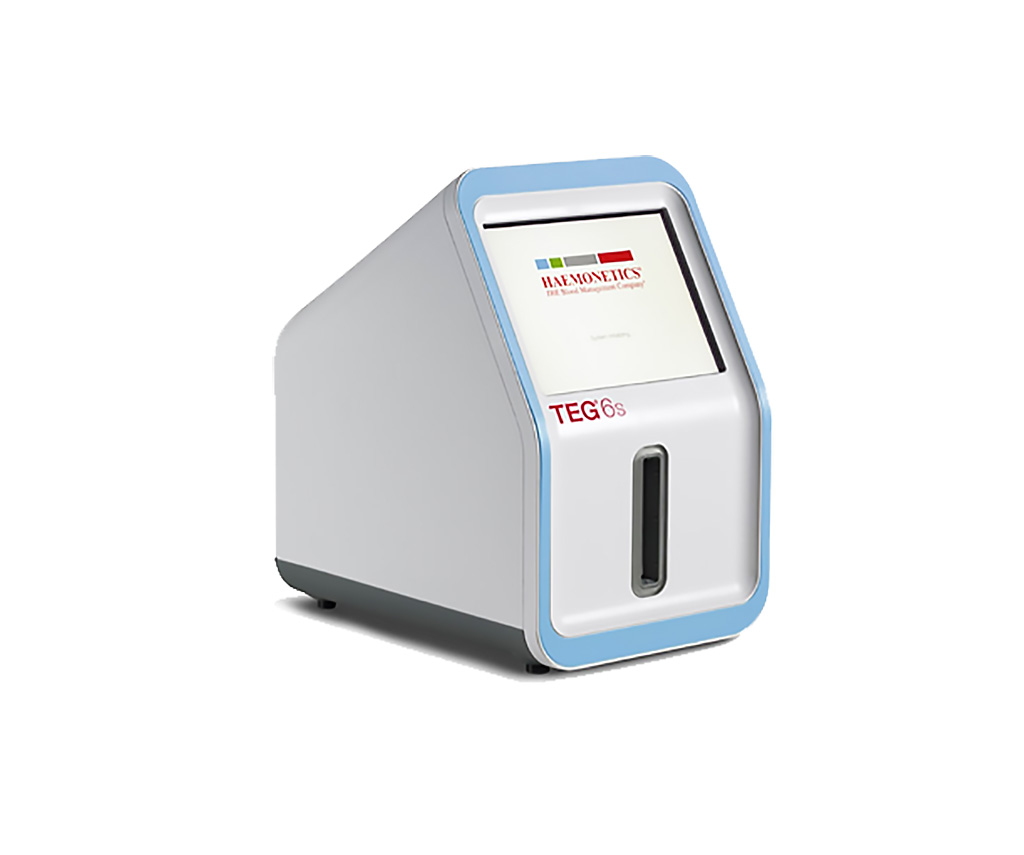
Image: The TEG 6s system provides rapid, comprehensive and accurate identification of an individual’s hemostasis condition in a laboratory or point-of-care setting (Photo courtesy of Haemonetics Corporation).
Medical scientists at the Shanghai Jiao Tong University School of Medicine (Shanghai, China) enrolled in a study a total of 41 patients with new‐onset SLE who had not undergone treatment were enrolled, and 56 healthy individuals were included as controls. Blood samples were collected using 18G needles and vacutainer tubes containing ethylenediaminetetraacetic acid (EDTA) (for complete blood cell count) and 3.2% trisodium citrate (for TEG and coagulation analyses). Moreover, 24‐hour urine collection was performed in a clean dry container.
Complete blood counts were obtained using an automated hematology analyzer DXH800 (Beckman Coulter, Brea, CA, USA). The reference range for PLT count was 101‐320 × 109/L. Routine coagulation screening assays, including PT, aPTT, fibrinogen (Fg), thrombin time (TT), d‐dimer (DD), and fibrinogen/fibrin degradation products (FDP), were performed in all the patients using an automated coagulometer CS5100 (Sysmex Corporation, Kobe, Japan). Lupus anticoagulant (LAC) status was examined using ACL‐TOP700 (Instrumentation Laboratory, Bedford, MA, USA). Blood clot formation and stability were evaluated via TEG tests using a thromboelastography analyzer (Haemonetics Corporation, Braintree, MA, USA).
The team reported that there was a significant difference in the TEG reaction time and TEG achievement of clot firmness between the groups. Moreover, these parameters were correlated with the lupus anticoagulant levels, platelet count, 24‐hour urinary total protein quantity, and systemic lupus erythematosus disease activity index ((SLEDAI). The TEG parameters were correlated with other clinical and laboratory data, such as LAC status, PLT level, and urinary total protein (UTP) and SLEDAI values. Patients with positive LAC status, higher PLT levels, UTP >500 mg/24 hours and higher SLEDAI values are known to have a greater risk of thrombosis.
The authors concluded that they have demonstrated the prospective value of TEG in evaluating hypercoagulability in patients with SLE. The study was published on December 16, 2019 in the Journal of Clinical Laboratory Analysis.
Related Links:
Shanghai Jiao Tong University School of Medicine
Beckman Coulter
Sysmex Corporation
Instrumentation Laboratory
Haemonetics Corporation