Routine Blood Parameters Predict Invasive Aspergillosis Prognosis
By LabMedica International staff writers
Posted on 19 Nov 2019
Aspergillosis occurs in chronic or acute forms which are clinically very distinct. Most cases of acute aspergillosis occur in patients with severely compromised immune systems, e.g. those undergoing bone marrow transplantation. Symptoms include fever, chills, shock, delirium, seizures, and blood clots.Posted on 19 Nov 2019
Acute invasive aspergillosis occurs when the immune system fails to prevent Aspergillus spores from entering the bloodstream via the lungs. Without the body mounting an effective immune response, fungal cells are free to disseminate throughout the body and can infect major organs such as the heart and kidneys. The patient may develop kidney failure, liver failure (causing jaundice), and breathing difficulties and death can occur quickly.
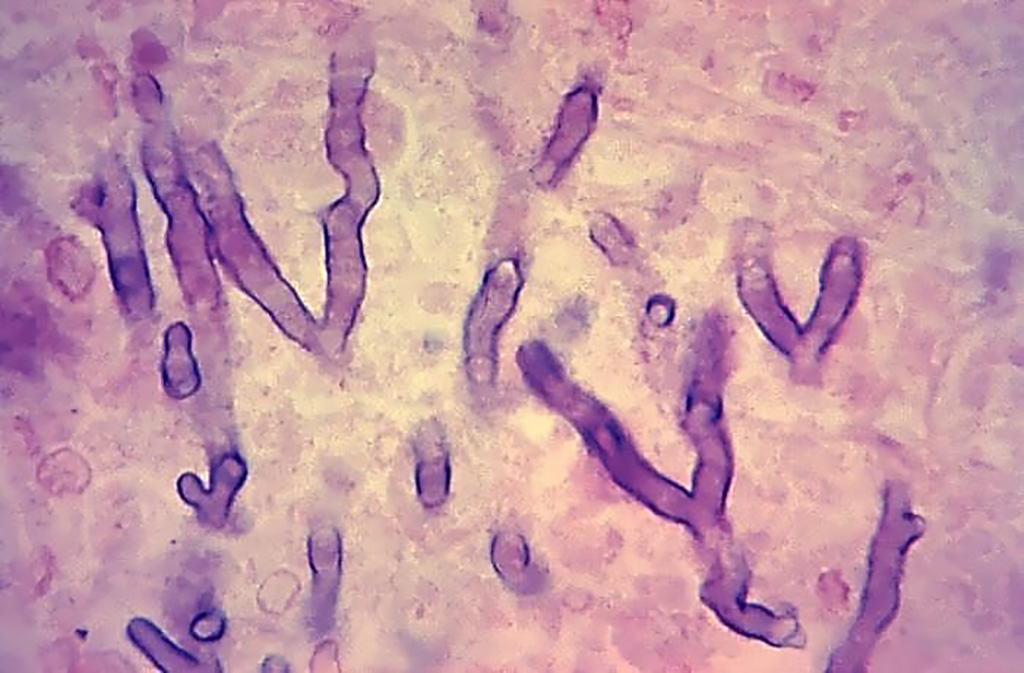
Image: Photomicrograph of a hematoxylin-eosin-stained human lung tissue specimen, harvested from a pulmonary aspergillosis patient. The histopathologic changes indicate the presence of Aspergillus sp. fungal organisms. Note the branching hyphae amongst the lung tissue (Photo courtesy of the Armed Forces Institute of Pathology).
A large team of scientists working with the National University of Singapore (Singapore) performed a post-hoc secondary analysis of two multicenter randomized trials. The Global Comparative Aspergillosis Study (GCA, N=123) and the Combination Antifungal Study (CAS, N=251) constituted the discovery and validation cohorts respectively. The outcome measures were response to treatment and survival to 12 weeks. Interval platelet, galactomannan index (GMI) and C-reactive protein (CRP) levels prior and during anti-fungal treatment were analyzed.
The investigators reported that the 12-week survival was 70.7% and 63.7% for the GCA and CAS cohorts respectively. In the GCA cohort, every 10×109/L platelet count increase at week 2 and 4 improved 12-week survival odds by 6-18% (Odds ratio [OR] 1.06-1.18). Survival odds also improved 13% with every 10 mg/dL CRP drop at week 1 and 2 (OR 0.87). In the CAS cohort, week 2 platelet count was also associated with 12-week survival with 10% improved odds for every 10×109/L platelet increase (OR, 1.10). A GMI drop of 0.1 units was additionally found to increase the odds of treatment response by 3% at the baseline of week 0 (OR 0.97). Week 2 platelet and CRP levels performed better than GMI on ROC analyses for survival (area under ROC curve 0.76, 0.87 and 0.67 respectively). A baseline platelet count higher than 30×109/L clearly identified patients with > 75% survival probability.
The authors concluded that higher serial platelets were associated with overall survival while GMI trends were linked to invasive aspergillosis treatment response. Routine and simple laboratory indices may aid follow-up of response in invasive aspergillosis patients. The study was published on October 24, 2019 in the journal Clinical Microbiology and Infection.
Related Links:
National University of Singapore













