New Method Rapidly Monitors Sickle Cell Disease
By LabMedica International staff writers
Posted on 26 Jun 2019
Sickle cell disease (SCD) is a hereditary disorder that affects red blood cells, distorting their natural disc shape into a crescent moon or "sickle" shape. Normal red blood cells move freely through small vessels throughout the body to deliver oxygen. With sickle cell disease, the misshapen red blood cells become hard and sticky, making it difficult for them to move through blood vessels.Posted on 26 Jun 2019
Sickle cell disease affects millions of people of many nationalities throughout the world, including both children and adults. A major challenge in managing the disease is the tremendous pain that patients endure from chronic and acute pain episodes called pain crisis. Unfortunately, these pain episodes are unpredictable and patients never know when or where these episodes will take place.
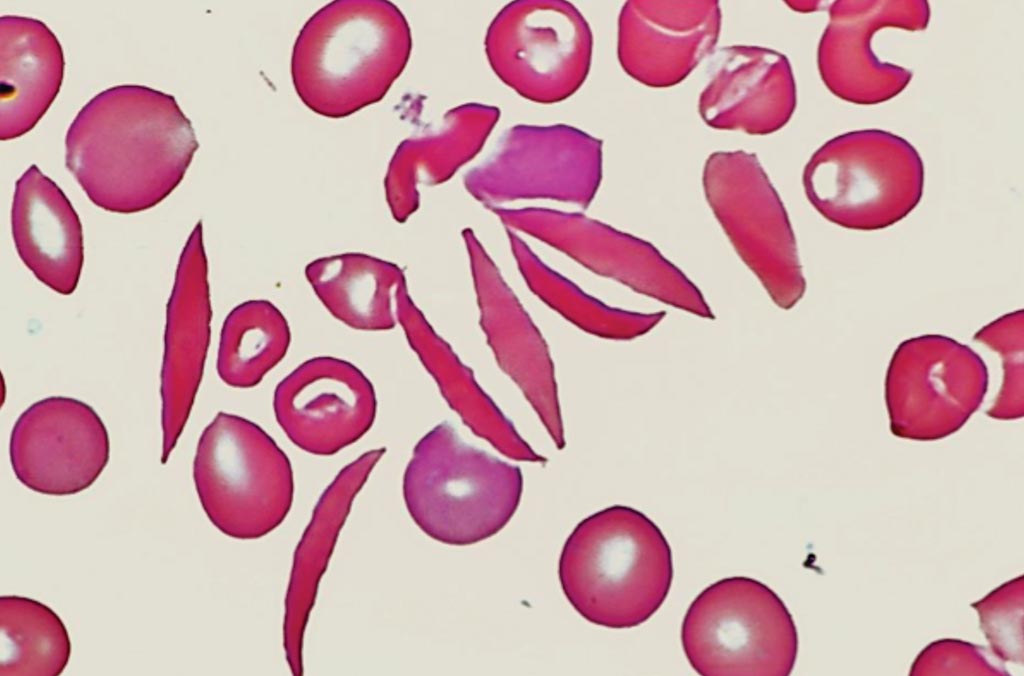
Image: A peripheral blood film from a patient with sickle cell disease (Photo courtesy of Venngage).
Bioengineers at the Florida Atlantic University (Boca Raton, FL, USA) and their hematologist colleague have developed a rapid and reliable new method to continuously monitor sickle cell disease using a microfluidics-based electrical impedance sensor. This novel technology can characterize the dynamic cell sickling and unsickling processes in sickle blood without the use of microscopic imaging or biochemical markers. The team collected five blood samples from individuals with SCD. A normal blood sample was obtained from a local blood bank and used as a control in the study. All samples were stored at 4 °C and tested within two weeks of collection.
Normalized impedance of all the five samples during the first hypoxia session were compared, allowing the scientists to identify intersample variations. The difference in sickling behavior was substantial. The team also established the correlations between the in vitro measurements and the patients' hematological parameters, such as the levels of sickle hemoglobin (HbS) and fetal hemoglobin (HbF). These findings show a potential clinical relevance because it serves as a proof-of-concept of electrical impedance as a label-free, biophysical marker of cell sickling events as well as a sensitive tool for probing the dynamic cellular and subcellular processes beyond the optical microscopy. The developed electrical impedance sensor may potentially be used for assessing vaso-occlusion risk, disease severity, and therapeutic treatment in sickle cell disease.
Sarah E. Du, PhD, an assistant professor and senior author of the study said, “The combination of electrical impedance measurement and on-chip hypoxia control provides a promising method for rapid assessment of the dynamic processes of cell sickling and unsickling in patients with sickle cell disease. In addition, electrical impedance measurement is naturally quantitative, real-time, and offers a convenience in direct or indirect contact with the samples of interest, allowing integrations to microfluidics platform and optical microscopy.” The study was published on May 14, 2019, in the journal ACS Sensors.
Related Links:
Florida Atlantic University














