Peripheral Blood Flow Cytometry Classifies Pediatric Acute Leukemia
By LabMedica International staff writers
Posted on 25 Feb 2019
Historically, flow cytometry performed on the bone marrow aspirate (BMFC) has been the standard for the immunophenotypic characterization of acute leukemia. Recent data have demonstrated the high sensitivity and specificity of peripheral blood flow cytometry for the diagnosis of pediatric leukemia.Posted on 25 Feb 2019
Peripheral blood flow cytometry (PBFC) represents a less invasive approach to the immunophenotyping of the leukemic clone, which can also facilitate a quicker diagnosis and the opportunity to subsequently perform concurrent central venous access device placement, lumbar puncture with intrathecal chemotherapy administration, and bone marrow biopsy, if necessary, under a single anesthetic.

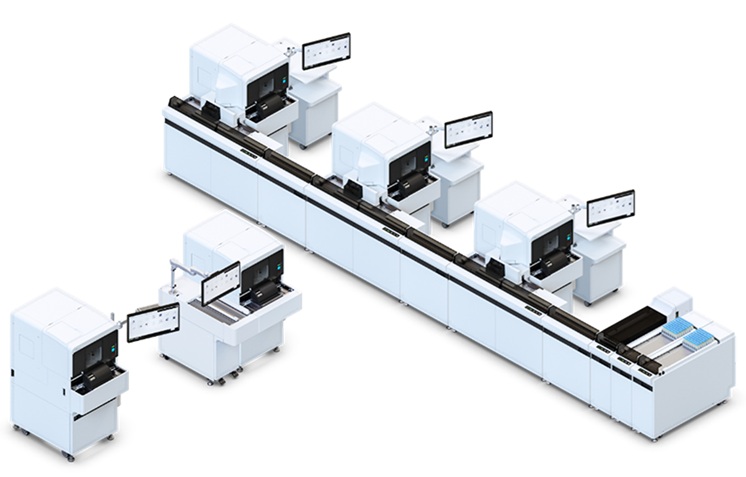
Image: The FACSCalibur flow cytometer used to immunophenotype pediatric leukemia (Photo courtesy of Becton Dickinson).
Medical laboratory scientists at St. Jude Children's Research Hospital (Memphis, TN, USA) collected peripheral blood and BM samples were collected in preservative‐free heparin or EDTA. Cells were washed twice in phosphate‐buffered saline and labeled with various combinations of monoclonal antibodies conjugated to fluorochromes directed against surface antigens or isotype‐matched nonreactive monoclonal antibodies. The samples were processed and analyzed using four or eight color stained cell preparations with FACSCalibur or FACSCanto II flow cytometers with FACSDiva software. A minimum of 20,000 cells per tube were counted. A diagnostic minimal residual disease (MRD) panel was also implemented.
The team identified 290 PBFC samples with concurrent BM evaluation. Based on the final immunophenotypic classification, the cases were distributed as follows: 108 B‐lymphoblastic leukemia (B‐ALL), 57 T‐lymphoblastic leukemia (T‐ALL), 116 acute myeloid leukemia (AML), and nine mixed‐phenotype acute leukemia (MPAL). Among all cases, five had a diagnostically significant discrepancy between PBFC and BM evaluation. In three cases, the immunophenotype by PBFC was consistent with early T‐cell precursor ALL (ETP‐ALL), whereas BM evaluation demonstrated MPAL. Two cases were suspicious for acute megakaryoblastic leukemia (AMKL) and MPAL, T/myeloid by PBFC, but were diagnosed as B‐ALL and T‐ALL in the BM.
The authors concluded that immunophenotypic classification by PBFC is accurate in more than 98% of all cases of pediatric leukemia with the rare exceptions of suspected ETP‐ALL, MPAL, and AMKL. These PBFC diagnoses should be confirmed with BM immunophenotyping. The study was published in the January 2019 issue of the journal Pediatric Blood & Cancer.
Related Links:
St. Jude Children's Research Hospital