Early Stage Breast Cancer Recurrence Linked to High Leukocyte Ratio
By LabMedica International staff writers
Posted on 23 Mar 2016
A high ratio of two types of immune system cell is linked to an increased risk of disease recurrence after a diagnosis of early stage breast cancer and the findings might guide future treatment and monitoring strategies, if prospective studies confirm the link.Posted on 23 Mar 2016
Breast cancer is a commonly diagnosed malignancy and the leading cause of cancer death in women worldwide and despite the widespread adoption of adjuvant treatments having resulted in improved survival, nearly 20% of patients with breast cancer still suffer from recurrence of disease.
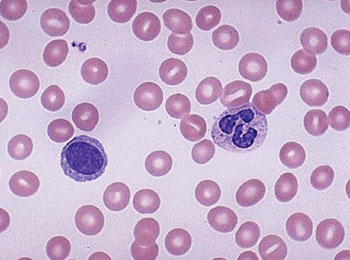
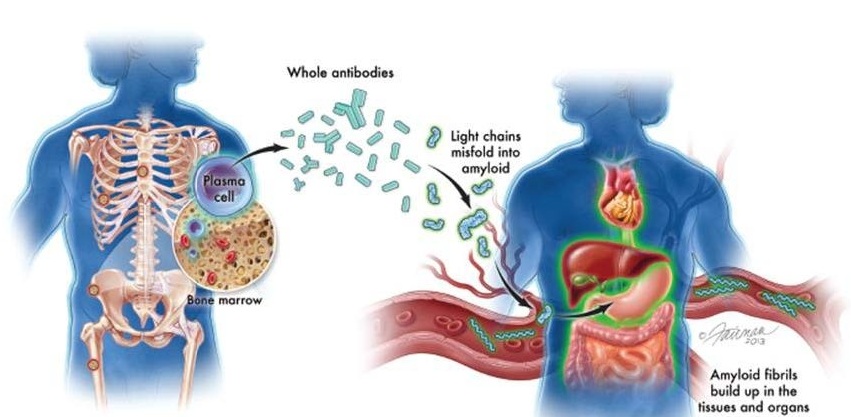
Image: Blood smear showing a segmented neutrophil and a mature lymphocyte with a single large nucleus (Photo courtesy of the University of Utah Medical School).
Scientists at the Second University of Naples School of Medicine (Caserta, Italy) carried out a retrospective study of A total of 300 female patients with histologically proven early (T1–2, N0–1, non-metastatic) breast cancer treated from July 1999 to June 2015. The following data were collected: age, menopausal status, histological tumor type, tumor size, tumor-node-metastasis stage, and degree of histological differentiation, expression of estrogen and/or progesterone receptor, human epidermal growth factor receptor (HER2) status, Ki67 levels, recurrence rate and distant metastasis–free survival (DMFS) rates.
The ratio of neutrophils to lymphocytes (NLR) ranged from 0.21 to 30.00 (mean 2.67±2.52, median 2.09) in the 300 patients. A significant NLR increase was observed only with T2 stage cancer, and NLR had the ability to distinguish between relapsing and non-relapsing patients. On the basis of their blood counts taken after diagnosis, but before treatment, 134 of the women had a low NLR of 1.97 or lower and 166 had a high NLR above 1.97. After 15 years, cancer had returned in another part of the body in 37 (12%) of the women. Women with a low NLR fared better at each of the subsequent check-ups at 1, 3, 6, 9, 12, and 15 years, with, respectively, 100%, 98.9%, 91.7%, 82.7%, 82.7%, and 82.7% of them free of recurrence. This compares with comparable figures of 99.4%, 94.3%, 84.5%, 69.2%, 66%, and 51.4% at the same time points in those with a high NLR.
The authors concluded that despite looking apparently simple, the relationship between NLR and outcome in patients with cancer is probably a complex and multifactorial process that is still poorly understood. In simple terms, a high NLR may reflect the key role of systemic inflammation in enhancing angiogenesis (formation of new blood vessels), tumor growth, and development of metastasis. The study was published on March 7, 2016, in the journal ESMO Open.
Related Links:
Second University of Naples School of Medicine