Newborn Screening Improves Early Detection and Treatment of SCID
By LabMedica International staff writers
Posted on 19 Aug 2014
Children born with severe combined immune deficiency (SCID), the so-called "bubble boy" disease, have the best chance of survival if they undergo a hematopoietic stem cell transplant as soon after birth as possible.Posted on 19 Aug 2014
The development of widespread screening of newborns for SCID and reports indicating a survival advantage for children with SCID who receive transplants in the first few months of life, have raised questions regarding immediate treatment.
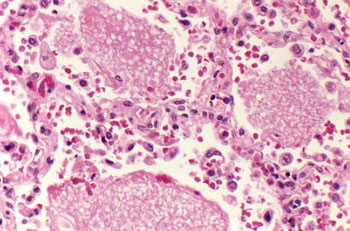
Image: Histopathology of a lung showing alveolar spaces containing exudates characteristic of infection with Pneumocystis jirovecii (Photo courtesy of Dr. Edwin P. Ewing, Jr).
A collaborative network of institutions in North America was formed to conduct rigorous multicenter studies addressing critical questions in the treatment of SCID. A retrospective analysis of data from 240 infants with classic SCID who received hematopoietic-cell transplants at 25 Primary Immune Deficiency Treatment Consortium (PIDTC) institutions during a 10-year period was carried out at the Dana-Farber Cancer Institute (Boston, MA, USA). Of the 285 infants who met the criteria for SCID, the 240 infants with classic SCID, on the basis of an absolute T-cell count of less than 300/mm3 and an absence of T-cell responses to mitogens, who had undergone allogeneic hematopoietic-cell transplantation, were included in the study.
In addition to patient age, the analysis finds that infection status at the time of transplant and donor source had the strongest impact on transplant outcomes, which is five-year survival and successful immune system reconstitution. Data gained from newborn screening suggest that SCID, while still rare, is twice as common as once thought. Infections were documented before transplantation in 171 of the 240 infants (71%), of whom 106 (62%) remained infected at the time of transplantation. Although bacteria and Pneumocystis jirovecii were the most common causes of infection, infections with DNA viruses or respiratory viruses were more likely to be active rather than resolved at the time of transplantation.
Children who underwent transplant before 3.5 months of age had excellent survival, regardless of donor source or infection status, as did patients transplanted with the stem cells of a matched sibling donor, long recognized as the gold standard of transplant. Children outside that age group also had very good survival regardless of donor source, sibling, parent, or unrelated donor, as long as the patient did not have an active infection at the time of transplant. The effect on survival of donor type and pre-transplant conditioning was only discernible in actively infected patients.
Sung-Yun Pai, MD, the lead author of the study, said, “Survival is much, much better if infants undergo transplant before they turn three-and-a-half months old and before they contract any SCID-related infections. The best way to identify patients that early when there is no family history of SCID is through newborn screening. This study accomplishes several things. First, it creates a baseline with which to compare patient outcomes since the advent of newborn screening for SCID. Second, it provides guidance for clinicians regarding the use of chemotherapy conditioning before transplantation. Third, it highlights the relative impacts of infection status and patient age on transplant success.” The study was published on July 31, 2014, in the New England Journal of Medicine (NEJM).
Related Links:
Dana-Farber Cancer Institute













