BPA Linked to Prostate Cancer, May Serve as Important Biomarker
By LabMedica International staff writers
Posted on 18 Mar 2014
New findings show that levels of bisphenol A (BPA) in men’s urine could be a marker of prostate cancer and that even low levels of BPA exposure can cause cellular changes in both non-malignant and malignant prostate cells.Posted on 18 Mar 2014
The study from a team at the Cincinnati Cancer Center (Cincinnati, OH, USA) provides the first evidence that urinary BPA levels may help predict prostate cancer (PrCa) and that cell-cycle disruption through exposure to low-dose BPA may be a cause of PrCa development.
Human exposure to BPA is ubiquitous. It is used to make hard, clear (polycarbonate) plastic and epoxy resins, and is common in many food product containers. Exposure has been linked to neurological defects, diabetes, cardiovascular disease, obesity, immune disorders, reproductive dysfunctions, and a number of cancers, including breast and prostate. Absorption through skin, inhalation, and ingestion from contaminated food and water are the major forms of exposure.
"As an endocrine disruptor that mimics estrogen and thyroid hormones, BPA also acts as a metabolic and immune disruptor,” said Shuk-mei Ho, PhD, director of the Cincinnati Cancer Center, and professor at the UC College of Medicine; "The adverse health effects of BPA are extensive, and studies in animals have proven this.” “However, human studies linking BPA exposure to heightened cancer risk are limited,” she continued, "Our study examined the association between urinary BPA levels and PrCa, and assessed the effects of BPA on the initiation of centrosome abnormalities as an underlying mechanism promoting PrCa formation.”
In the study, BPA was assessed for 60 urology patients using urine samples. Higher levels of BPA were found in PrCa patients than in non-PrCa patients—5.74 µg/g versus 1.43 µg/g (creatine adjusted), and the difference was even more significant in patients less than 65 years of age. Serum PSA levels were not different between patients with and without PrCa, but a trend (small patient size) toward a negative association between urinary BPA and serum PSA was noticed in PrCa patients and not in non-PrCa patients.
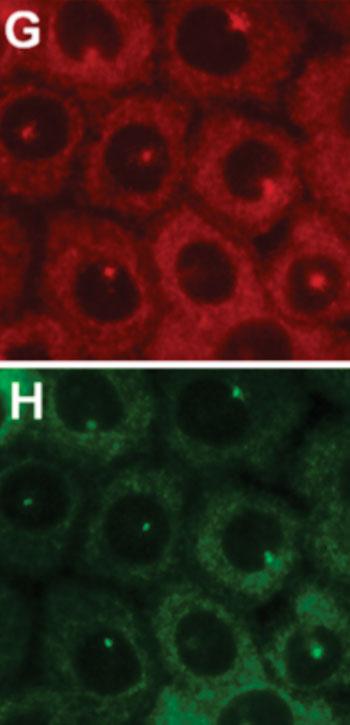
Additionally, normal and cancerous prostate cell lines were examined in vitro using immunofluorescence to visualize the distribution of the target molecule and to look at centrosomal abnormalities and growth patterns. "Exposure to low doses of BPA increased the percentage of cells with centrosome amplification 2- to 8-fold,” said Prof. Ho; "BPA is not a recognized carcinogen, and questions surrounding the mechanism behind the positive correlation of BPA exposure with PrCa have arisen. Several studies have shown that centrosome amplification is a major contributing factor to chromosomal mutation in human tumors. We [...] found that treatment with BPA increased the number of cells with abnormal centrosomes.” So, disruption of the centrosome duplication cycle by low-dose BPA may contribute to prostate carcinogenesis and cancer progression.
The findings, published by Tarapore P. et al., March 3, 2014, in the journal PLOS One, provide strong evidence that urinary BPA level is an independent prognostic marker for prostate cancer. The study also warns (though currently based on a small sample size) that BPA exposure may lower serum PSA levels in tests for monitoring prostate cancer patients.
Related Links:
Cincinnati Cancer Center












.jpg)