Circulating Angiogenic Factor Levels Predict Hypertensive Disorders of Pregnancy
Posted on 16 Nov 2022
Preeclampsia is the most common hypertensive disorder associated with pregnancy. The severe form of the disease can lead to dangerously high blood pressure, organ failure, vision loss or even stroke. It affects approximately 5% of pregnant women and is a leading cause of maternal and fetal death and serious illness.
Currently, the only cure for preeclampsia is delivery. A test indicating that a preterm patient, a woman who has completed less than 37 weeks of pregnancy, is likely to develop severe disease could help optimize care. Prior studies suggest that preeclampsia is characterized by angiogenic factor imbalance. Levels of soluble fms-like tyrosine kinase 1 (sFlt-1) and/or placental growth factor (PlGF), both angiogenic placental proteins, may be used to predict, diagnose, and prognosticate women with a suspicion of preeclampsia.
A large team of Medical Scientists led by those at Cedars-Sinai Medical Center (Los Angeles, CA, USA), prospectively measured across 18 USA centers, the ratio of serum soluble fms-like tyrosine kinase 1 (sFlt-1) to placental growth factor (PlGF) in pregnant women hospitalized between 23 and 35 weeks of gestation. The primary outcome was predicting preeclampsia with severe features (sPE), and secondary outcomes included predicting adverse outcomes within two weeks. The prognostic performance of the sFlt-1: PlGF ratio was assessed by using a derivation/validation design. Between 2019 and 2021, the enrolled 1,014 women at one of 18 USA hospitals with a singleton pregnancy and a hypertensive disorder of pregnancy.
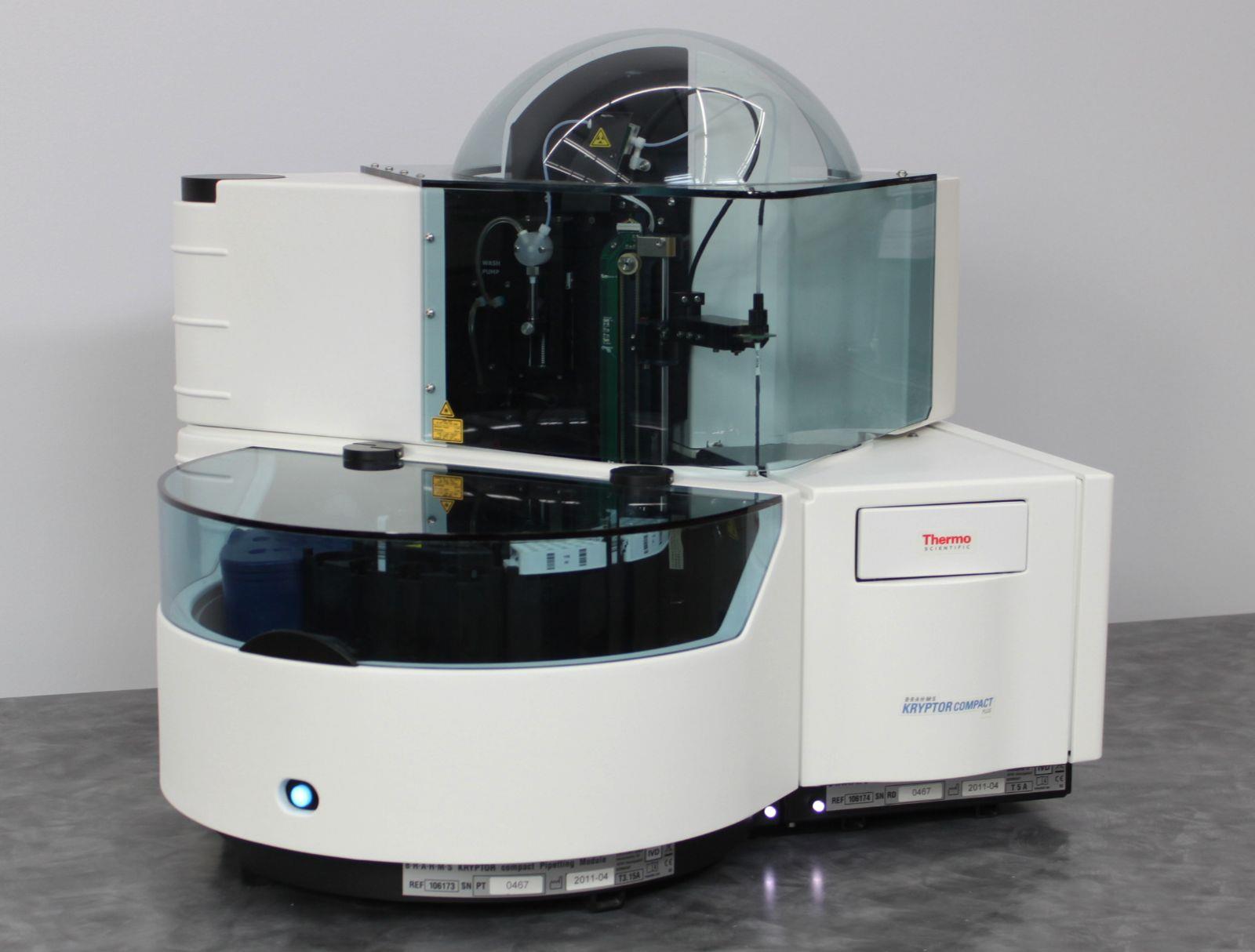
Serum samples were stored at –20 °C or lower within five hours of venipuncture. Specimens were routinely batch-shipped from sites to Cedars-Sinai Medical Center where sFlt-1 and PlGF levels (both in picograms per milliliter [hence the ratio is unitless]) were measured in a blinded fashion on an automated sandwich immunoassay platform: BRAHMS PlGF and sFlt-1 (KRYPTOR; Thermo Fisher Scientific, Henningsdorf, Germany). These assays are CE-marked and have been validated in pregnant populations.
The investigators reported that of the total of 1,014 pregnant women that were evaluated; 299 were included in the derivation cohort and 715 in the validation cohort. In the derivation cohort, the median sFlt-1: PlGF ratio was 200 (interquartile range, 53 to 458) among women who developed sPE compared with 6 (interquartile range, 3 to 26) in those who did not. The discriminatory ratio of ≥40 was then tested in the validation cohort and yielded a 65% positive and a 96% negative predictive value for the primary outcome. The ratio performed better than standard clinical measures (area under the receiver-operating characteristic curve, 0.92 versus <0.75 for standard-of-care tests). Compared with women with a ratio <40, women with a ratio ≥40 were at higher risk for adverse maternal outcomes (16.1% versus 2.8%; relative risk, 5.8).
Sarah Kilpatrick, MD, PhD, co-senior author of the study, said, “This test was significantly better than all the standard-of-care markers for preeclampsia with severe features. It predicted with over 90% accuracy whether the patient would develop preeclampsia with severe features or not, while the usual markers were accurate less than 75% of the time."
The authors concluded that in women with a hypertensive disorder of pregnancy presenting between 23 and 35 weeks of gestation, measurement of serum sFlt-1: PlGF provided stratification of the risk of progressing to sPE within the coming fortnight. The study was published on November 9, 2022 in the journal NEJM Evidence.
Related Links:
Cedars-Sinai Medical Center
Thermo Fisher Scientific