Ammonia Predicts Prognosis in Hepatitis B Virus‐Related Liver Failure
By LabMedica International staff writers
Posted on 24 Sep 2020
Acute‐on‐chronic liver failure (ACLF) is the rapid deterioration of liver function in chronic liver disease often associated with the development of serious complications such as hepatorenal syndrome and hepatic encephalopathy within a short period of time. Posted on 24 Sep 2020
Hepatic encephalopathy (HE) is a common feature of acute liver failure and has been reported to be associated with poor outcomes. Ammonia is thought to be central to the pathogenesis of HE, but its role in hepatitis B virus‐related acute‐on‐chronic liver failure (HBV‐ACLF) is unclear.

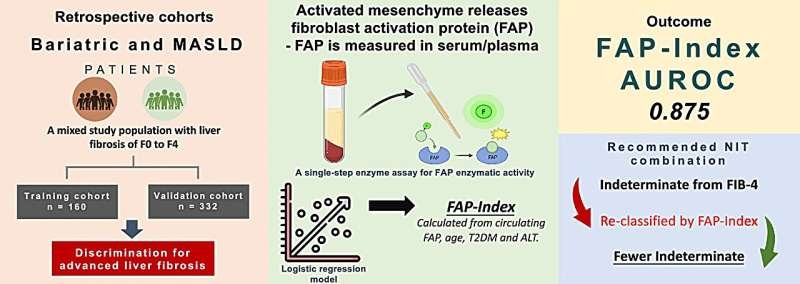
Image: The Vitros 350 clinical chemistry system (Photo courtesy of Ortho Clinical Diagnostic).
Clinical Laboratorians at the Zhejiang University (Hangzhou, China) recruited all 127 patients with HBV‐ACLF, defined as total bilirubin (TBIL) ≥ 205 μmol/L and international normalized ratio (INR) ≥ 1.5 according to COSSH‐ACLF criteria, who were treated at their institution between July 2018 and February 2020 for a retrospective study.
Laboratory parameters included total protein, albumin, alanine aminotransferase, aspartate aminotransferase, creatinine, TBIL, arterial ammonia, INR, white blood cell count, platelet count, and blood urea nitrogen. Arterial ammonia was estimated within 24 hours of admission using a Vitros 350 dry chemistry system (Ortho Clinical Diagnostic, Rochester, NY, USA) in heparinized plasma.
The scientists reported that the median ammonia level at enrollment was 55.0 (interquartile range, 36.0‐76.0) and 77 patients (60.6%) had high ammonia at the time of admission. Ammonia level was found to be positively correlated to model for end-stage liver disease (MELD) score and COSSH‐ACLF score. In the study population, there were 61 patients with cirrhosis and 66 patients without cirrhosis. No significant difference between the two groups except that the age of the cirrhosis group was higher than that of the non‐cirrhosis group.
Among the 127 participants, 87 survived and 40 died, representing a 28‐day mortality rate of 31.5%. The mean MELD score, TBIL, INR, white blood cell count, ammonia, and COSSH‐ACLF score were higher among non‐surviving participants; however, the mean age, gender ratio, total protein, albumin, alanine aminotransferase, aspartate aminotransferase, creatinine, blood urea nitrogen, and platelet count were not significantly different between survivors and non‐survivors. Dividing patients according to the ammonia cut‐off value of 73 μmol/L revealed higher ammonia level to be associated with higher alanine aminotransferase, INR, mortality rate, COSSH‐ACLF score and MELD score.
The authors concluded that their results suggest that high ammonia level at admission is an independent factor for predicting short‐term mortality in patients with HBV‐ACLF. Therefore, ammonia levels may represent a therapeutic target for this condition. The study was published on September 11, 2020 in the Journal of Clinical Laboratory Analysis.