Relationship of Serum Cortisol and Serum Sodium Analyzed
By LabMedica International staff writers
Posted on 19 Jul 2017
Hyponatremia is the most common electrolyte disorder encountered by the clinical biochemist, and is associated with a significant mortality and hypernatremia is also a risk factor for mortality in critically ill patients.Posted on 19 Jul 2017
Adrenal insufficiency is an uncommon cause of hyponatremia, but one that should not be overlooked because an Addisonian crisis, once recognized, can be easily and safely treated with fluid replacement and corticosteroid. Clinical practice guidelines on hyponatremia advise that primary or secondary adrenal insufficiency should always be considered as a potential cause of hyponatremia.

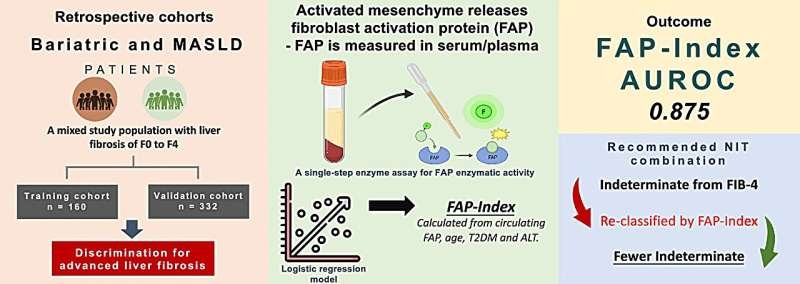
Image: The Advia Centaur XP immunoassay analyzer (Photo courtesy of Siemens Healthcare).
Medical laboratory scientists at the Leeds General Infirmary (Leeds, UK) defined severe hyponatremia as a sodium concentration equal to or less than 120 mmol/L and severe hypernatraemia was defined as a sodium concentration equal to or greater than 150 mmol/L. The reference range for serum cortisol in a morning sample at the Leeds Teaching Hospitals NHS Trust is 150 to 600 nmol/L. Data was gathered on samples where both serum sodium and cortisol that had been requested from the laboratory information management system for 23 months (January 1, 2013, until November 30, 2014).
Serum sodium and cortisol were measured on Advia 1800 or 2400 and Centaur XP analyzers respectively. Analysis of the data from 3,268 patients revealed a trend showing higher cortisol concentrations in patients who were severely hypo- or hypernatremic. The median cortisol concentration for patients with sodium equal to or less than 110 mmol/L was 856 nmol/L, and there was a gradual decrease in cortisol over the sodium range equal to or less than 110 to 150 mmol/L. Patients with sodium equal to or greater than 151 mmol/L had a median cortisol of 725 nmol/L, and 42% of the 978 patients with serum sodium of less than or equal to 120 mmol/L had serum cortisol measured within two weeks, of whom 1.7% were diagnosed with adrenal insufficiency.
The authors concluded that despite the relative rarity of endocrine causes of hyponatremia, adrenal insufficiency should remain an important consideration in the clinical workup of the hypernatremic patient due to the severe consequences of failure to treat with glucocorticoid replacement and volume repletion. The dataset shows rising cortisol in response to hypo- or hypernatremia, in keeping with the stress response to illness. The data show that adrenal insufficiency is a rare cause of hyponatremia, which may be overlooked. The full study will be published in the August 2017 issue of the journal Practical Laboratory Medicine.
Related Links:
Leeds General Infirmary