Combined Molecular Test Distinguishes Benign Pancreatic Lesions
By LabMedica International staff writers
Posted on 05 Jul 2017
When performed in tandem, two molecular biology laboratory tests distinguish, with near certainty, pancreatic lesions that mimic early signs of cancer but are completely benign. Serous cystic neoplasms (SCNs) have no malignant potential, but can mimic the following premalignant mucinous cystic lesions: mucinous cystic neoplasm and intraductal papillary mucinous neoplasm (IPMN).Posted on 05 Jul 2017
Patients with SCN undergo imaging or other surveillance every six months to spot changes indicative of cancer, or they undergo an operation to remove part of the gland as a precaution because SCN are difficult to find using standard diagnostic methods. More than 60% of SCN are not predicted preoperatively and 50% to 70% are missed or incorrectly diagnosed on radiology scans.
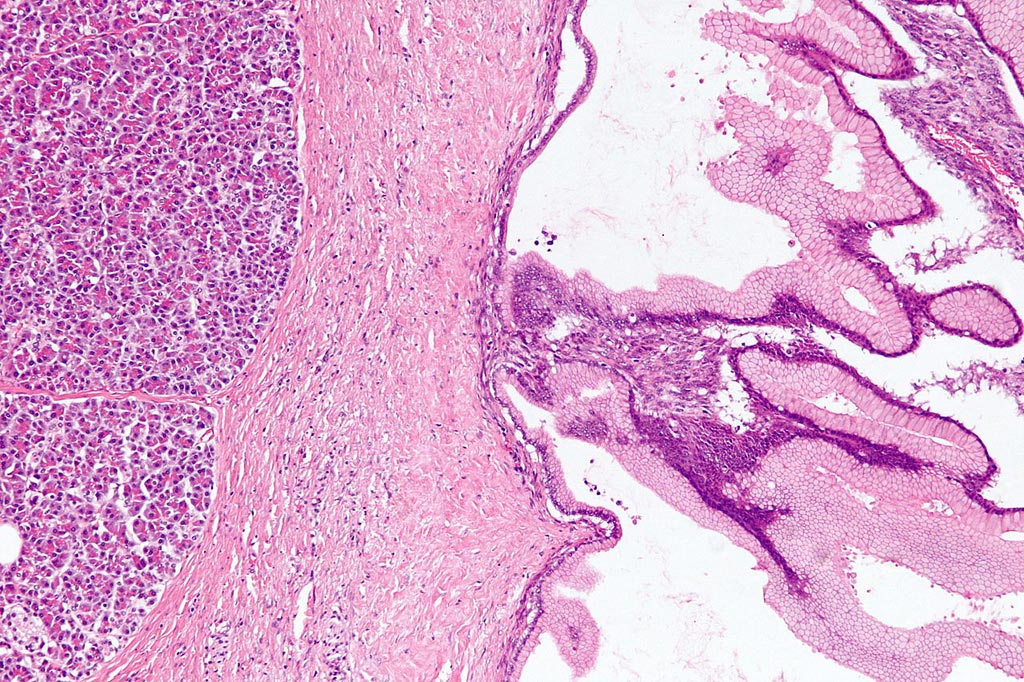
Image: Benign pancreatic mucinous cystic neoplasm (Photo courtesy of Wikipedia).
Medical scientists at the Indiana University School of Medicine (Indianapolis, IN, USA) included in their study 149 patients who underwent an operation to remove a pancreatic cystic lesion and 26 of these patients had SCN. The diagnosis of each surgical specimen was confirmed by pathologic examination, and samples of pancreatic fluid from all patients were tested for Vascular endothelial growth factor A (VEGF-A) and Carcinoembryonic antigen (CEA) according to testing protocols for enzyme-linked biochemical analysis of fluids (ELISA).
The team discovered that tests for each of these proteins in pancreatic cyst fluid accurately distinguished SCN from other types of pancreatic lesions. In the present study, VEGF-A with a threshold of greater than 5,000 pg/mL alone, singled out SCN with a sensitivity of 100% and specificity of 83.7%, and CEA with a threshold of equal to or less than10 ng/mL, had a 95.5% sensitivity and 81.5% specificity. Together, however, the tests approached the gold standard of pathologic testing: The combination had a sensitivity of 95.5% and specificity of 100% for SCN. Authors of the study concluded that results of the VEGF-A/CEA test could have prevented 26 patients from having unnecessary surgery.
C. Max Schmidt, MD, PhD, FACS, a professor of surgery and biochemical/molecular biology and senior study author, said, “Every day, surgeons follow patients who have pancreatic cysts that have no risk of cancer but are still worrisome. They perform surgery or conduct diagnostic tests just to make sure they're not wrong. With VEGF-A and CEA, we believe we may have invented a test that can help that group of patients who don't have a risk of cancer get off the testing cycle and avoid surgery which, in and of itself, has a risk of mortality or complications.” The study was published in the July 2017 issue of the Journal of the American College of Surgeons.
Related Links:
Indiana University School of Medicine










 (3) (1).png)