Microneedle Delivery of Beta-Cells Avoids Host Immune Rejection
By LabMedica International staff writers
Posted on 28 Mar 2016
A novel skin patch filled with living insulin-secreting beta cells was shown to regulate glucose levels in a mouse diabetes model for up to 10 hours while avoiding adverse immune responses.Posted on 28 Mar 2016
Attempts to treat diabetes by transplanting beta-cells have not been particularly successful, since most transplants are rejected and the medications used to suppress the immune system interfere with the activity of beta cells and insulin.
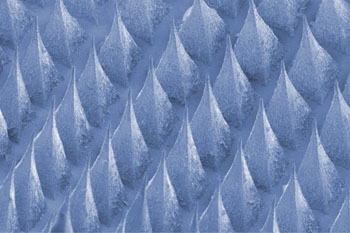
Image: A scanning electron microscopic (SEM) image of the microneedle-array beta-cell patch (Photo courtesy of Dr. Zhen Gu, University of North Carolina).
Investigators at the University of North Carolina (Chapel Hill, USA) and North Carolina State University (Raleigh, USA) devised a way to protect foreign beta cells from attack by the immune system.
They described in the March 1, 2016, online edition of the journal Advanced Materials an innovative microneedle (MN)-based cell therapy device that enabled glucose-responsive regulation of the insulin secretion from exogenous pancreatic beta-cells without implantation.
The device was a synthetic patch comprising hundreds of biocompatible microneedles, each packed with thousands of alginate encapsulated beta-cells and culture media. When applied to the skin, the microneedles pierced capillaries and dermal blood vessels, forming a connection between the internal environment and the external cells of the patch that enabled diffusion of insulin from the patch into the skin.
Results revealed that one microneedle patch quickly reduced the blood-sugar levels (BGLs) of chemically induced type-1 diabetic mice and stabilized BGLs at a reduced level for over 10 hours. Repeated administration of the patch did not result in excess doses of insulin and did not induce hypoglycemia. Rather, application of a second patch extended the life of the treatment to 20 hours.
“This study provides a potential solution for the tough problem of rejection, which has long plagued studies on pancreatic cell transplants for diabetes,” said senior author Dr. Zhen Gu, assistant professor of biomedical engineering at the University of North Carolina. “Plus, it demonstrates that we can build a bridge between the physiological signals within the body and these therapeutic cells outside the body to keep glucose levels under control.”
Related Links:
University of North Carolina
North Carolina State University