ADLM’s New Coagulation Testing Guidance to Improve Care for Patients on Blood Thinners
Posted on 06 Nov 2025
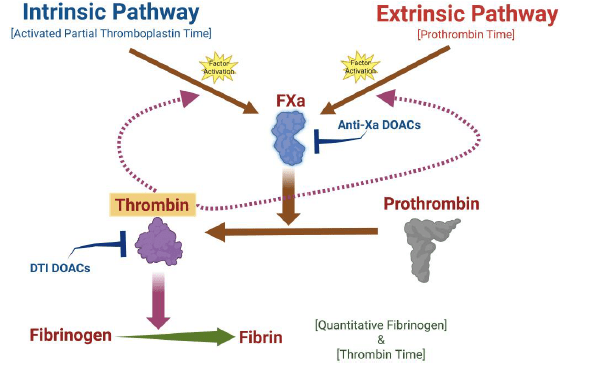
Direct oral anticoagulants (DOACs) are one of the most common types of blood thinners. Patients take them to prevent a host of complications that could arise from blood clotting, including stroke, deep vein thrombosis, and pulmonary embolism. Unlike older anticoagulants, DOACs do not require regular monitoring with coagulation testing, which measures the blood's ability to clot.
However, there are still other scenarios in which patients on DOACs might need coagulation testing. This includes when they're experiencing heavy bleeding, being tested for a possible clotting disorder, or before an urgent or elective surgery to ensure bleeding is controlled. In these instances, selecting the right testing approach can be tricky, since DOACs directly interact with the same clotting factors at play in certain coagulation tests. Now, a group of experts has created a guidance document on this topic that organizes and simplifies key points from a large body of previously published research and medical reports.
The Association for Diagnostics & Laboratory Medicine (ADLM, formerly AACC, Washington, DC, USA) has issued expert guidance on coagulation testing in patients taking blood thinners that have the potential to interfere with these tests. By helping clinicians and laboratory medicine professionals to navigate the complex testing scenarios that arise with these patients, the new guidelines will help ensure that they still receive accurate diagnoses and effective treatment.
The document recommends labs and healthcare providers to avoid clot-based testing for patients on DOACs when possible. The guidance details the tests that are and are not susceptible to interference from these drugs so that labs and healthcare professionals can make an informed decision on which tests to use for these patients. In scenarios where clot-based testing is necessary, the document recommends labs and clinicians to mitigate DOACs' potential effects by treating blood samples before testing with agents that neutralize those effects, temporarily discontinuing DOAC treatment before a coagulation test, or temporarily switching a patient to a low-molecular weight heparin. In order for any of these strategies to be effective, the document recommends laboratory medicine professionals and clinicians to communicate effectively, as the perspectives and expertise of both are needed to ensure patients get the appropriate tests and treatments.
"Clinicians ordering coagulation testing for patients taking DOACs should approach these scenarios thoughtfully, as this requires discretion to determine appropriate and optimal timing for testing," wrote the document authors Drs. Lindsay A.L. Bazydlo, Maximo J. Marin, Anna E. Merrill, Louise M. Man, Olajumoke O. Oladipo, and Neil S. Harris. "Communication and collaboration with the laboratory leadership and staff is strongly suggested prior to testing. The laboratory medical director can provide guidance to the clinical team on current methodologies and how to interpret results for patients on DOACs."
Related Links:
ADLM













