Blood Test Could Predict Best Treatment for Lung Cancer
By LabMedica International staff writers
Posted on 09 Dec 2016
A blood test could predict how well small-cell lung cancer (SCLC) patients will respond to treatment. In most patients with SCLC, a metastatic, aggressive disease, the condition is initially chemosensitive, but then relapses with acquired chemoresistance.Posted on 09 Dec 2016
In a minority of patients with SCLC, however, relapse occurs within three months of initial treatment; in these cases, disease is defined as chemorefractory. The molecular mechanisms that differentiate chemosensitive from chemorefractory disease are currently unknown.
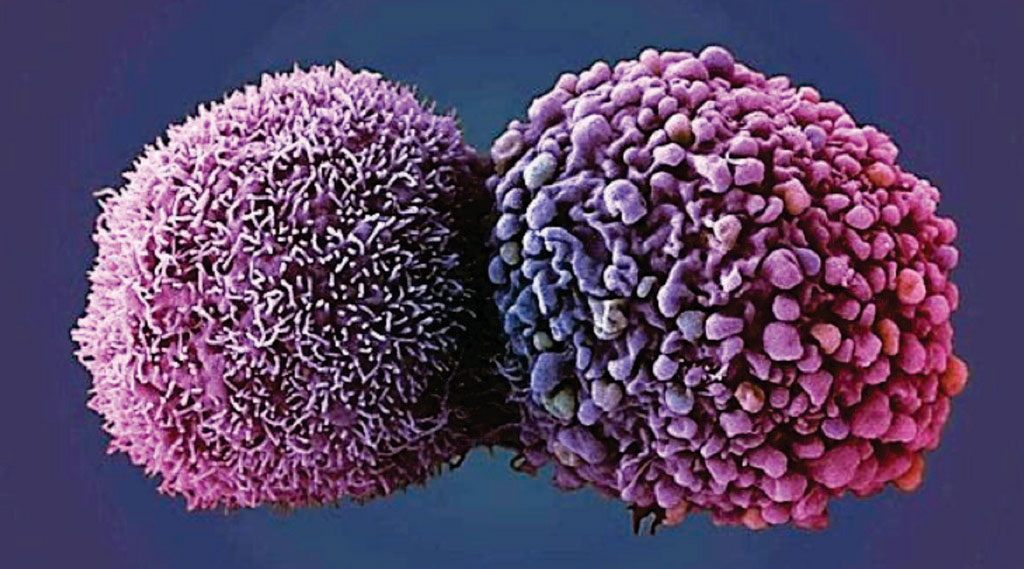
Image: A colorized scanning electron micrograph (SEM) of two lung cancer cells (Photo courtesy of Anne Weston/Cancer Research UK).
Scientists, based at the Cancer Research UK Manchester Institute at The University of Manchester (UK) examined copy-number aberrations (CNAs) in circulating tumor cells (CTCs) from pretreatment SCLC blood samples to identify genetic features that distinguish chemosensitive from chemorefractory disease. After analysis of 88 CTCs isolated from 13 patients (training set), they generated a CNA-based classifier that they validated in 18 additional patients (testing set, 112 CTC samples) and in six SCLC patient-derived CTC explant tumors.
The classifier correctly assigned 83.3% of the cases as chemorefractory or chemosensitive. Furthermore, a significant difference was observed in progression-free survival (PFS) between patients designated as chemorefractory or chemosensitive by using the baseline CNA classifier. Notably, CTC CNA profiles obtained at relapse from five patients with initially chemosensitive disease did not switch to a chemorefractory CNA profile, which suggests that the genetic basis for initial chemoresistance differs from that underlying acquired chemoresistance.
Caroline Dive, PhD, a professor and the lead investigator, said, “Our study reveals how blood samples could be used to anticipate how lung cancer patients may respond to treatments. Unfortunately, we have very few treatment options for patients with SCLC, and none at all for those whose cancer is resistant to chemotherapy. By identifying differences in the patterns of genetic faults between patients, we now have a starting point to begin to understand more about how drug resistance develops in patients with this aggressive form of lung cancer.” The study was published on November 21, 2016, in the journal Nature Medicine.
Related Links:
Cancer Research UK Manchester Institute













