Groundbreaking Immune Approach Targets Humans Instead of Bacteria
By LabMedica International staff writers
Posted on 18 Oct 2016
Staphylococcal and streptococcal infections affect millions of individuals each year and they are a leading cause of sepsis and account for many cases of pneumonia and post-surgical infections.Posted on 18 Oct 2016
The ability of staphylococcal and streptococcal bacteria to cause disease is due to numerous virulence factors, among which a group called Superantigens play a prominent role. Several dozen superantigens are highly lethal in humans and are critical contributors to sepsis and progression to toxic shock.
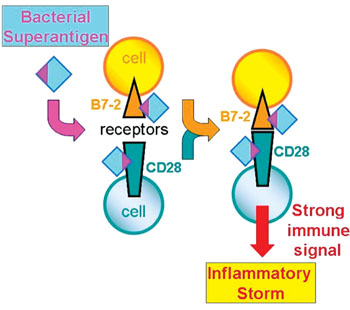
Image: A diagram of the newly discovered mechanism of action of the bacterial superantigen toxins: Superantigens bind to both B7-2 and CD28, the major costimulatory receptors expressed on human immune cells. This binding enhances B7-2/CD28 receptor engagement, thereby inducing a powerful immune signal that evokes a harmful inflammatory storm (Photo courtesy of Professor Raymond Kaempfer).
Scientists at the Hebrew University-Hadassah Medical School (Jerusalem, Israel) developed describe a novel host-oriented therapeutic approach for preventing lethal immune responses. With major implications for medicine, the novel approach is both broad-acting and impervious to bacterial antibiotic resistance. While the inflammatory immune response is essential to protecting humans against viruses and bacteria, superantigen toxins cause an exaggerated response, called an immune storm, that can do a great deal of damage in the body and can result in multiple organ failure. Even with currently available treatment strategies, most of these diseases have high mortality rates. Complicating treatment of these bacterial infections are multi-drug resistant strains.
A normal immune response is mediated by an antigen through the joining of cells through well-known receptors on their surface, a process that is helped by the so-called "costimulatory" receptors. Unexpectedly, the superantigen strongly promotes the interaction between the major costimulatory receptors, B7-2 and CD28, and this turns out to be critical for its ability to elicit an immune storm. Formation of the costimulatory axis was already known to be important for a full immune response, but the present findings propel this axis to the foreground as a key bottleneck.
The investigators now show that in order to enhance B7-2/CD28 receptor engagement, superantigen molecules bind directly to both receptors. By binding not only CD28 but also its co-ligand B7-2 directly, superantigens potently enhance the B7-2/CD28 interaction, inducing thereby T-cell hyperactivation. Bacterial superantigens thus induce the pathogenic immune storm by strongly enhancing formation of the B7-2/CD28 costimulatory axis. Insight into this mechanism led the scientists to design new peptides, snippets of the human B7-2 receptor protein that powerfully block the binding of a superantigen to its costimulatory receptor targets, and thereby protect against lethal toxic shock, as they showed in animals. Each peptide mimics a small part of the site in B7-2 where the superantigen must bind. Acting as a decoy of the intact receptor, such a peptide will bind the superantigen toxin and thereby block its access to the receptor needed for toxicity.
Raymond Kaempfer, PhD, a professor of Molecular Biology and lead author of the study said, “Rather than targeting the bacterial pathogens, which can then mutate to develop antibiotic resistance, host-oriented therapeutics have the advantage of remaining effective even against infections with antibiotic-resistant strains. This is because before the pathogens can cause severe disease, they must also pass through the same receptor bottleneck in the immune response, which we can block effectively.” The study was published on October 4, 2016, in the journal Proceedings of the National Academy of Science.
Related Links:
Hebrew University-Hadassah Medical School