Bacteria Links Crohn's Disease to Spondyloarthritis
By LabMedica International staff writers
Posted on 22 Feb 2017
Peripheral spondyloarthritis (SpA) is a common extraintestinal manifestation in patients with active inflammatory bowel disease (IBD) characterized by inflammatory enthesitis, dactylitis, or synovitis of nonaxial joints.Posted on 22 Feb 2017
Patients with Crohn's disease, a type of IBD that causes abdominal pain and diarrhea can also experience joint pain. In Crohn's disease, which affects about 800,000 Americans, the immune system can attack not only the bowels, but the musculoskeletal system as well, leading to spondyloarthritis, a painful condition that affects the spine and joints.
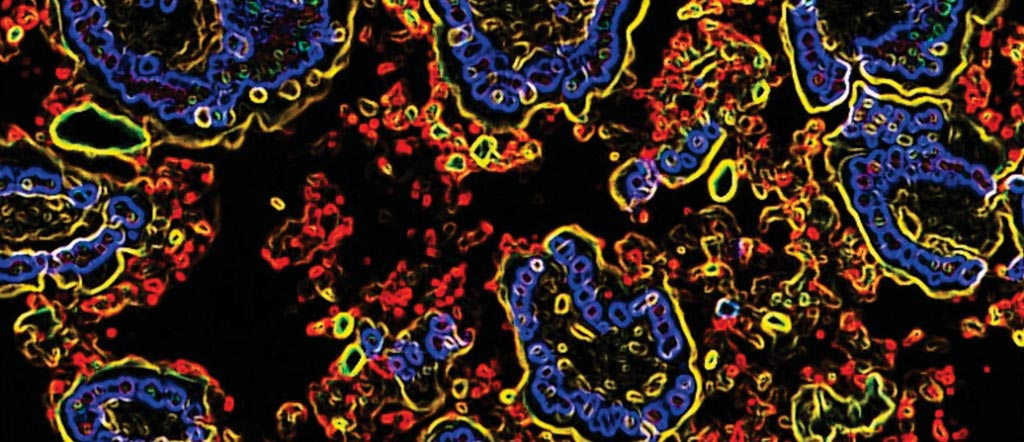
Image: Escherichia coli bacteria (red), which are abundant in the immunoglobulin-A-coated microbiota of patients with a Crohn\'s disease-associated condition called spondyloarthritis, promote systemic inflammation. The blue circular structures depict the nuclei of cells called epithelial cells (Photo courtesy of Dr. Kenneth Simpson, Cornell University).
A large team of scientists working in conjunction with those at Weill Cornell Medicine College used fecal samples from patients with IBD to identify bacteria in the gut that were coated with antibodies called immunoglobulin-A (IgA) that fight infection. Using flow cytometry, in which fluorescent probes are used to detect IgA-coated bacterial species, the team discovered that IgA-coated Escherichia coli were abundant in fecal samples from patients with both Crohn's disease and spondyloarthritis.
The investigators used both patient samples and mouse models and then linked these bacteria to cells that help regulate inflammation, known as Th17 cells, in people with autoimmune disorders. The investigators found that patients with Crohn's disease and spondyloarthritis had higher levels of Th17 cells, and that a protein called interleukin-23 (IL-23) triggers their activity. E. coli isolates from CD-SpA–derived IgA-coated bacteria were similar in genotype and phenotype to an adherent-invasive E. coli (AIEC) pathotype. By modeling the increase in mucosal and systemic TH17 immunity they observed in CD-SpA patients, colonization of interleukin-10–deficient or K/BxN mice with CD-SpA–derived E. coli lead to more severe colitis or inflammatory arthritis, respectively.
Randy Longman, MD, PhD, a gastroenterologist and mucosal immunologist and a principal investigator of the study said, “In IBD therapy, this is a step toward precision medicine; to be able to clinically and biologically characterize a subtype of disease and then select the medicine that would best fit the patient with this type of inflammation. The results of this innovative study will start to inform our decision of which of our available medications will give the best chance of helping the individual patient.” The study was published on February 8, 2017, in the journal Science Translational Medicine.













