Prognostic Tool Identified for Newly Diagnosed Multiple Myeloma
By LabMedica International staff writers
Posted on 29 Dec 2016
The bone marrow (BM) microenvironment contains numerous cell types, including immunosuppressive tumor-associated macrophages (TAM), that promote the growth and survival of multiple myeloma (MM) cells.Posted on 29 Dec 2016
Emerging evidence suggests that the absolute monocyte count (AMC) in peripheral blood may reflect the level of TAM recruitment at the tumor site and its prognostic significance has been shown in other lymphoid malignancies. Absolute lymphocyte count (ALC) as a surrogate marker for host immune system has prognostic significance.
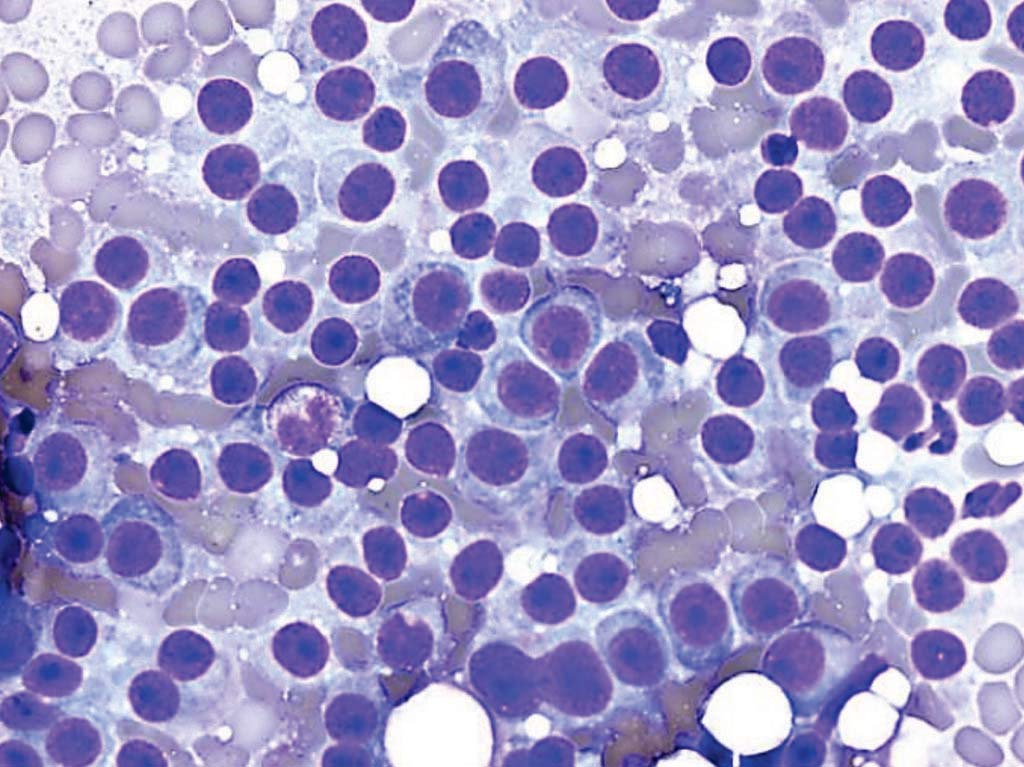
Image: A photomicrograph of bone marrow aspirate from a patient with multiple myeloma, showing numerous plasma cells, which can be recognized by the eccentric nucleus and perinuclear halo (Photo courtesy of Dr. Michael G. Bayerl).
A team of scientists led by those at University Hospitals Case Medical Center (Cleveland, OH, USA) investigated the prognostic significance of the ratio of ALC, as a surrogate of host immune status, to AMC, which reflects the MM-immune microenvironment, in predicting clinical outcome among newly diagnosed MM patients. The study included 372 MM patients diagnosed 2004-2014 who had complete blood count (CBC) differentials at diagnosis. The primary end-point of the study was progression free survival (PFS) calculated from the time of diagnosis.
The median patient age was 67.3 years (range: 30-92), 53% were male and 47% female. At the time of this analysis 92 patients (24%) had died, 75 (20%) of them was due MM. The median AMC, ALC and ALC/AMC ratio at diagnosis was 412 cells/µL, 1,461 cells/µL and 3.9, respectively. Neither ALC nor AMC was associated with different PFS or overall survival (OS). ALC/AMC as a continuous variable was identified as a predictor of PFS; hazard ratio (HR) = 0.62.The 236 patients with an ALC/AMC equal to or greater than 3.6 experienced a superior median PFS compared to the 136 patients with an ALC/AMC less than 3.6; Median PFS, 24 versus 43 months respectively. Low ALC, high AMC, and low ALC/AMC ratio were associated with poor prognostic factors such as high β2-microglobulin.
The authors concluded that myeloma patients with a higher ALC/AMC at diagnosis enjoyed a longer PFS (either as a continuous or dichotomized variable). Also, multivariate analysis demonstrated that patient with tumors that harbored del (17p) or t(4, 14) had low ALC/AMC ratio suggesting possible immunoparesis. The data potentially suggest the ALC/AMC ratio as a readily available surrogate marker to assess the relative strength of host immune system to myeloma-induced immunoparesis. The ratio can serve as a biomarker to stratify patients for future immunological therapies an also indicates that the host immune status should be carefully monitored. The study was presented at the 58th Annual Meeting of American Society of Hematology (ASH) held December 3-6, 2016, in San Diego, CA, USA.
Related Links:
University Hospitals Case Medical Center









 Analyzer.jpg)



