Successful Treatment of Enteritis Due to Newly Discovered Gene Mutation
By Michal Siman-Tov
Posted on 07 Dec 2016
Researchers report successful treatment of an adult patient with severe chronic autoimmune enteritis by using the drug Vedolizumab to target the effect on T-cell function of a mutation identified in the patient’s CTLA-4 gene. Vedolizumab may also help skin cancer patients with enteritis due to therapy with Ipilimumab.Posted on 07 Dec 2016
Over 300 different genetically determined immunodeficiencies have been identified so far. However, as genetic immunodeficiencies rarely occur, they often go unrecognized or are detected too late for effective treatment.
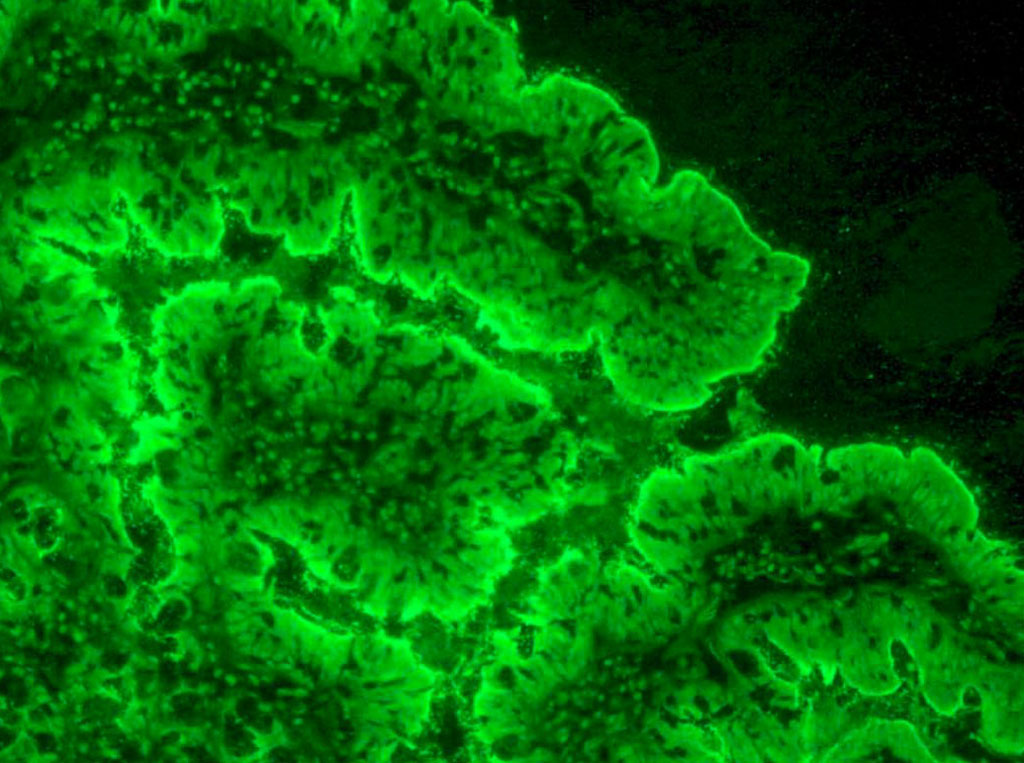
Image: Indirect immunofluorescence on a patient’s intestinal lining shows anti-enterocyte antibodies. Enterocytes are the cells of the intestinal lining (Photo courtesy of the NIH).
A team led by Mike Recher, professor at University of Basel (Basel, Switzerland) and University Hospital Basel, discovered the CTLA-4 gene mutation and that targeted therapy with Vedolizumab could successfully treat the patient. The patient had a rare mutation in the CTLA-4 protein found on the surface of T-cells. Normally, this protein prevents immune cells from attacking a patient’s own body. However, the mutation caused an autoimmune reaction where T-cells attacked the patient’s intestinal cells, causing chronic inflammation that resulted in the patient suffering from severe diarrhea and weight loss.
Initially, these unusual symptoms had led the cantonal hospital of Graubünden to refer the patient to the special clinic for immunodeficiency at the University Hospital Basel, where immunological investigations suggested a genetically determined dysregulation of the immune system. The new CTLA-4 gene mutation was discovered following subsequent analysis of the entire genome at the University Hospital Zurich. Further investigations showed that the mutation causes reduced CTLA-4 function, which led to increased infiltration of the intestinal mucosa by T-cells and therefore to chronic diarrhea.
Working with the gastroenterology department, the doctors opted for a therapy that uses a new drug from the monoclonal antibody group to prevent the T-cells from penetrating the intestinal mucosa. This drug, Vedolizumab, blocks a specific adhesion molecule on the T-cell surface and thereby inhibits immune cells from binding themselves to receptors present in the intestine, preventing the T-cells from penetrating the blood vessels in the intestinal tissue. This treatment produced the desired outcome: after 3 months, the patient’s chronic diarrhea had stopped completely.
Additionally, this work suggested that CTLA-4 inhibition could be used therapeutically to preventing diarrhea in patients with other diseases, such as when treating melanoma with the drug Ipilimumab, which works similarly to the CTLA-4 mutation in that T-cells are no longer properly inhibited and can more efficiently attack the malignant skin cancer cells. One side effect of Ipilimumab is autoimmune intestinal inflammation – analogous to that caused by the CTLA-4 mutation. It is possible that melanoma patients suffering from severe diarrhea due Ipilimumab will benefit from this new insight, which would open new therapeutic possibilities for Vedolizumab.
This case demonstrates the importance of precise diagnosis of the molecular causes of an illness in enabling targeted, personalized treatment. “In order to expand our knowledge in these areas, doctors in clinics and regional hospitals must be on the alert for unusual disease phenotypes and refer such patients to specialized university hospital clinics for further evaluation,” said Prof. Recher, “We also need clinical university centers that are closely linked to research laboratories.”
The study, by Navarini AA et al, was published online November 28, 2016, in the Journal of Allergy and Clinical Immunology.
Related Links:
University of Basel