Sickle Cell Trait Confounds Blood Sugar Readings
By LabMedica International staff writers
Posted on 23 Feb 2017
Sickle cell trait (SCT) is a genetic hemoglobin variant found in 8% to 10% of African-Americans and it occurs in people with one copy of the mutation because if they had two copies, that would result in sickle cell disease.Posted on 23 Feb 2017
Hemoglobin A1c (HbA1c) is a common blood biomarker used to measure blood sugar over time, but it may not perform as accurately among African-Americans with sickle cell trait and could be leading to a systemic underestimation of blood sugar control among that population.
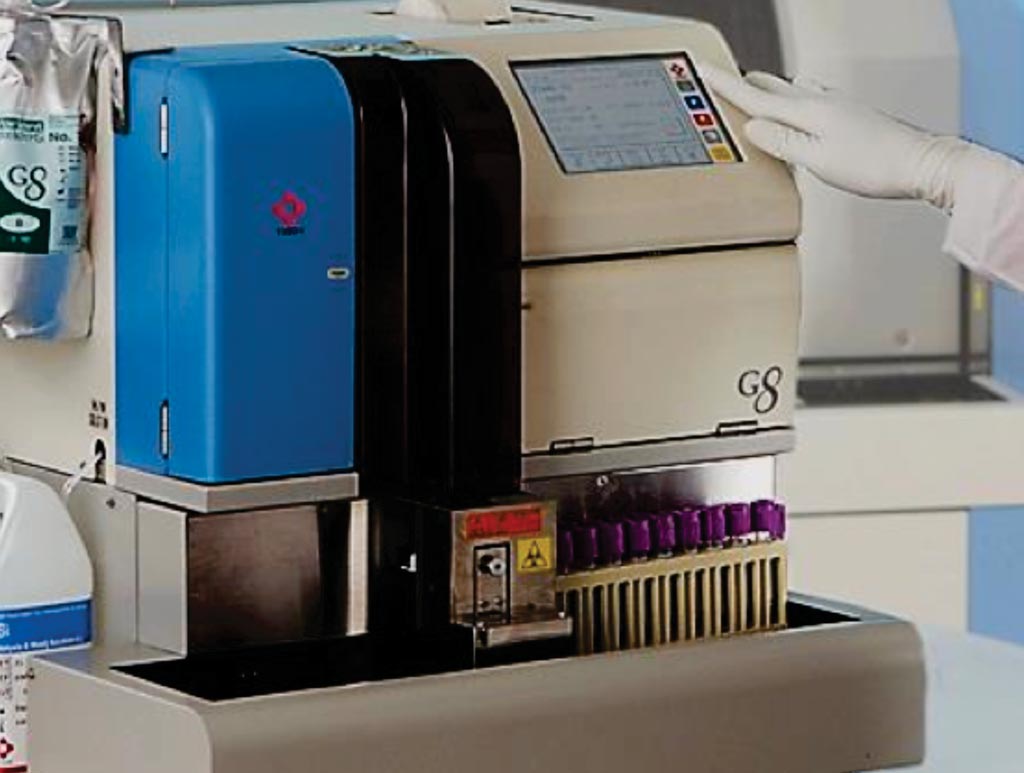
Image: The G8 HPLC analyzer for HbA1c measurement (Photo courtesy of Tosoh Bioscience).
A team of scientists led by those at the Brown University School of Public Health performed a retrospective cohort study on data from two studies and the analytic sample included 4,620 participants (mean age, 52.3 ±11.8 years; 2,835 women (61.3%); 367 (7.9%) with SCT) with 9,062 concurrent measures of fasting glucose and HbA1c. Analysis of the primary outcome was conducted using generalized estimating equations (GEE) to examine the association of SCT with HbA1c levels, controlling for fasting or 2-hour glucose measures.
Among all the patients included in the analysis, HbA1c readings came from either of two widely used, clinically accepted assays made by Tosoh Bioscience Inc. that rely on a process called high-performance liquid chromatography. In addition to those measures, the scientists also compared fasting and two-hour blood glucose and statistically controlled for demographic and medical factors, such as gender, age, body-mass index and whether diabetes had already been diagnosed and whether it was being treated.
The team found that using standard clinical HbA1c cutoffs resulted in identifying 40% fewer potential cases of prediabetes and 48% fewer potential cases of diabetes in people with SCT than in people without SCT. Meanwhile, when the scientists used other blood glucose measures as the diagnostic criteria, they found no significant difference in the likelihood of diabetes and prediabetes among patients with or without SCT. Current diagnostic thresholds for HbA1C are greater than 5.7% for prediabetes and greater than 6.5% for diabetes.
The authors of the study therefore recommend that practitioners following African-American patients whose HbA1c levels are within 0.3 percentage points of a diagnostic cutoff also consider using additional blood glucose measures. Gregory A.Wellenius, ScD, an associate professor of epidemiology and co-author of the study said, “The strengths of the study are that it's the largest sample size ever used, it's across two different studies with somewhat different populations, and it's a more thorough evaluation than prior studies.” The study was published on February 7, 2017, in the Journal of the American Medical Association (JAMA).